Electronic Visit Verification Policy Handbook
1000, Electronic Visit Verification Policy Handbook Introduction
Revision 21-1; Effective Nov. 1, 2021
The Electronic Visit Verification (EVV) Policy Handbook provides EVV standards and policy requirements that program providers and Financial Management Services Agencies (FMSAs) contracted with Texas Health and Human Services Commission (HHSC) and managed care organizations (MCOs) must follow. The EVV Policy Handbook also includes requirements for Consumer Directed Services (CDS) employers.
EVV standards and policy requirements do not replace or supersede program or licensure requirements. Program providers and FMSAs must follow all program and licensure rules and policies in addition to EVV policies.
The EVV Policy Handbook has EVV requirements for both HHSC and MCOs (the payers). Program providers and FMSAs must adhere to their individual contracts with HHSC or an MCO and contact the payer for questions on EVV and non-EVV requirements.
The requirements in this handbook apply to the programs and services identified in the HHSC Texas Administrative Code (TAC) Title 1, Part 15, Chapter 354, Subchapter O, RULE Section 354.4005, Applicability Code, Section Applicability.
1100 EVV Overview
Revision 21-1; Effective Nov. 1, 2021
A program provider, FMSA or CDS employer must use an EVV vendor system or an HHSC-approved EVV proprietary system to electronically document the delivery of an EVV service.
EVV is a computer-based system that electronically documents and verifies service delivery information, such as date, time, service type and location for certain Medicaid service visits.
An EVV system must capture the following data elements:
- The type of service provided
- The name of the recipient to whom the service is provided
- The date and times the provider began and ended the service delivery visit
- The location, including the address and geolocation, at which the service was provided
- The name of the service provider who provided the service
- Other information the commission determines is necessary to ensure the accurate adjudication of Medicaid claims
To ensure that EVV is used for all required services, HHSC or an MCO will not pay an EVV claim without a matching EVV visit transaction.
Texas HHSC determines when a program provider, FMSA or CDS employer must use EVV based on the services delivered. EVV is required for all programs and services listed in the Programs and Services Required to Use EVV document.
1200 State Laws and Texas Administrative Code
Revision 22-4; Effective Sept. 1, 2022
Texas law requires HHSC to implement an EVV program.
Program providers or FMSAs contracted with HHSC or an MCO must follow state law, TAC and associated policies established by HHSC when delivering Medicaid services.
Texas EVV statute and TAC include:
- Texas Government Code Section 531.024172
- Texas Administrative Code, Title, 1 Part 15, Chapter 354, Subchapter O
Live-in caregivers are not exempt from EVV requirements in Texas.
1300 Federal Law
Revision 21-1; Effective Nov. 1, 2021
The 21st Century Cures Act (the Cures Act), enacted by the U.S. Congress in Dec. 2016, added Section 1903(l) to the Social Security Act to require all states to use EVV.
The Cures Act requires the use of EVV for personal care services (PCS) provided under a State plan of the Social Security Act or under a waiver of the plan including sections 1905(a)(24), 1915(c), 1915(i), 1915(j), 1915(k) and Section 1115; and home health care services (HHCS) provided under 1905(a)(7) provided under a State plan of the Social Security Act or a waiver of the plan. This includes services delivered under the CDS option.
States must implement EVV by the following deadlines or risk a loss of federal Medicaid matching dollars:
- PCS by Jan. 1, 2020.
- Texas received approval for a one-year delay of the deadline to Jan. 1, 2021.
- HHCS by Jan. 1, 2023.
- Texas may apply for a one-year delay of the deadline to Jan. 1, 2024
Failure to implement EVV in accordance with the Cures Act will result in a reduction of federal Medicaid funding for Texas.
1400 Failure to use an EVV System
Revision 21-1; Effective Nov. 1, 2021
Program providers, FMSAs and CDS employers must ensure an approved EVV system is used to document the delivery of EVV-required services.
Failure to use an approved EVV system to document service delivery for required programs and services will result in denied or recouped EVV claims. Per the TAC Title, 1 Part 15, Chapter 354, Subchapter O, Rule Section 354.4009 HHSC and MCOs will not pay a claim for reimbursement unless the data from the EVV system corresponds with the claim line item and is consistent with an approved prior authorization.
Program providers and FMSAs who fail to use an EVV system may also be subject to contract actions, such as, but not limited to, corrective action(s) or contract termination. CDS employers who fail to use an EVV system may be subject to removal from the CDS option.
If the service provider or CDS employee fails to clock in and clock out of the EVV system, the program provider, FMSA or CDS employer must manually enter the visit into the EVV system. Manually entered visits will negatively impact EVV compliance.
In the event the EVV system is unavailable, the service provider or CDS employee must document service delivery information and submit the documentation to the program provider, FMSA or CDS employer for manual entry of an EVV visit.
Service delivery documentation should include:
- Program Provider, FMSA and CDS employer Name;
- Member First and Last Name
- Member Medicaid ID
- Services Delivered
- Date of the Visit
- Actual Time In and Actual Time Out
- Service provider First and Last Name
- Location of the Visit - in the home or in the community
Program providers, FMSAs and CDS employers must keep all service delivery documentation and manually enter EVV visits into the EVV system according to the service delivery documentation once the EVV system is operational or as otherwise instructed by HHSC.
1500 Resources and Communications
Revision 21-1; Effective Nov. 1, 2021
All program providers, FMSAs and CDS employers must sign up for GovDelivery to receive the most current news and alerts related to EVV.
Program providers, FMSAs and CDS employers can visit the HHSC EVV webpage to access the most up to date information such as:
- EVV News and Alerts
- Programs and services which require the use of EVV
- Statutes and rules governing EVV
- Service bill codes for EVV
- EVV contact information guide
- EVV training requirements and resources
1600 Key Terms
Revision 22-4; Effective Sept. 1, 2022
Key Terms are words regularly used throughout the EVV Policy Handbook. If a term is already defined in the handbook, the reference is provided below.
Auto-Verification (auto-verify) – An automatic process the EVV system performs to confirm an EVV visit transaction matches existing critical data elements and schedule data, if applicable, in the EVV system with no exceptions.
Business Day – Monday through Friday, except national or state holidays.
Consumer Directed Service (CDS) employer – Refer to 2800 CDS Employer and 16010 CDS Option Stakeholders.
Consumer Directed Services (CDS) option – A service delivery option in which a CDS employer employs and retains a service provider and directs the delivery of services.
Electronic Visit Verification (EVV) – Refer to 1100 EVV Overview.
EVV Aggregator – Refer to 6200 EVV Aggregator.
EVV Compliance Reviews – Refer to 10000 EVV Compliance Reviews.
EVV Claim – Documentation submitted to HHSC or an MCO for reimbursement of services required to use EVV.
EVV Portal – An online system established by HHSC that allows users to perform searches and view reports associated with visit data and EVV claim match results in the EVV Aggregator.
EVV proprietary system – Refer to 5000 EVV Proprietary System.
EVV system – An EVV vendor system or an EVV proprietary system used to electronically document and verify critical data elements related to the delivery of EVV services.
EVV System Administrator – A person appointed by a program provider or an FMSA to serve as the primary contact for administering access to an EVV system. Refer to 4130 Select an EVV System for more information.
EVV vendor system – Refer to 4110 EVV Vendor System.
EVV visit maintenance – Refer to 8000 Visit Maintenance.
EVV visit transaction – Refer to 6000 EVV Visit Transaction.
Exception – Refer to 8010 Required Visit Maintenance.
Financial management services agency (FMSA) – Refer to 2600 Financial Management Services Agency and 16010 CDS Option Stakeholders.
Member – Refer to 2700 Member and 16010 CDS Option Stakeholders.
Payer – Refer to 2100 Payers.
Program provider – Refer to 2500 Program Provider.
Reason Code Description and Reason Code Number – Refer to 9000 EVV Reason Code.
Service Delivery Documentation – Information written on paper or another format by the service provider when the EVV system is unavailable to document the delivery of service. Refer to 1400 Failure to use an EVV System for more information.
Service provider (or CDS employee) – A person who provides an EVV service to a member and is employed by or contracted with either a program provider or CDS employer. Note: Service providers who are contracted directly with HHSC or an MCO as a program provider must meet applicable EVV requirements for service providers and program providers.
Service Responsibility Option (SRO) – A service delivery option where a member or LAR selects, trains, and provides daily management of a service provider, while the fiscal, personnel and service back-up plan responsibilities remain with the program provider.
Signature Authority – A person who has legal authority to sign contracts and make transactional decisions.
2000, EVV Stakeholders
Revision 21-1; Effective Nov. 1, 2021
The following EVV stakeholders must meet all state and federal EVV requirements:
- Payers (HHSC and MCOs)
- Texas Medicaid and Healthcare Partnership (TMHP)
- EVV vendors
- Program providers delivering services under the agency option
- FMSAs
- Medicaid members and SRO participants
- CDS employers
2100 Payers
Revision 22-4; Effective Sept. 1, 2022
Payers are responsible for paying Medicaid claims, administering the EVV program and enforcing EVV requirements. In Texas, the payers are HHSC and the MCOs.
Payer responsibilities include, but are not limited to:
- Following state and federal requirements when processing claims for services required to use EVV
- Developing EVV policies, processes and procedures
- Providing EVV policy training to program providers, FMSAs and CDS employers
- Conducting EVV compliance reviews of program providers, FMSAs and CDS employers
HHSC requires EVV for Medicaid personal care services authorized by the following HHSC programs:
- Long-term Care (LTC) Fee-for-Service (FFS)
- Acute Care FFS
- Managed Care
HHSC is the payer for LTC and acute care services administered by the state, known as FFS. Acute care payments are made by TMHP on behalf of HHSC.
LTC FFS
| Programs |
|---|
| Community Attendant Services (CAS) |
| Family Care (FC) |
| Community Living Assistance and Support Services (CLASS) Waiver |
| Primary Home Care (PHC) |
| Deaf Blind Multiple Disability (DBMD) Waiver |
| Home and Community-based Services (HCS) Waiver |
| Texas Home Living (TxHmL) Waiver |
Acute Care FFS
| Programs |
|---|
| Personal Care Services (PCS) |
| Community First Choice (CFC) |
| Youth Empowerment Services (YES) Waiver |
| Home and Community-based Services-Adult Mental Health (HCBS-AMH) Waiver |
MCOs are the payers for managed care services.
Managed Care
| Programs |
|---|
| STAR Health, including MDCP covered services |
| STAR+PLUS |
| STAR+PLUS Home and Community Based Services (HCBS) |
| STAR Kids, including MDCP covered services |
| STAR+PLUS Medicare-Medicaid Plan (MMP) |
2200 Texas Medicaid and Health Care Partnership
Revision 21-1; Effective Nov. 1, 2021
Texas Medicaid and Healthcare Partnership (TMHP) is the state’s claims administrator and is responsible for the Medicaid Management Information System (MMIS) where the EVV Aggregator resides. TMHP is also responsible for the EVV Portal, the EVV vendor pool and coordinates all data exchange for EVV systems.
TMHP responsibilities include, but are not limited to, the following:
- Processing claims for EVV services, including forwarding claims to MCOs
- Paying claims for Acute Care FFS on behalf of HHSC
- Managing the EVV Aggregator and EVV Portal
- Selecting and managing the approved EVV vendors on behalf of HHSC
- Training on the EVV Portal
The TMHP EVV webpage has more information.
2300 EVV Vendors
Revision 22-4; Effective Sept. 1, 2022
An EVV vendor is contracted with the state’s claims administrator to provide a cost free EVV system for program providers and FMSAs.
EVV vendor responsibilities include, but are not limited to:
- Adhering to all HHSC EVV vendor business rules for system operation and functionality
- Following all EVV requirements described in:
- The EVV Policy Handbook
- Texas Administrative Code, Title 1, Part 15, Chapter 354, Subchapter O
- Texas Government Code Section 531.024172 or its successors
- Supporting multiple clock in and clock out methods
- Providing EVV system training and technical support
Refer to 4100 EVV System Selection for more information.
2400 EVV Proprietary System Operator
Revision 22-4; Effective Sept. 1, 2022
An EVV Proprietary System Operator (PSO) is a program provider or FMSA that uses an HHSC-approved EVV proprietary system.
EVV PSO responsibilities include, but are not limited to:
- Adhering to all HHSC EVV Business Rules for Proprietary Systems
- Following all EVV requirements described in:
- The EVV Policy Handbook
- Texas Administrative Code, Title 1, Part 15, Chapter 354, Subchapter O
- Texas Government Code Section 531.024172 or its successors
- Supporting one or more clock in and clock out methods
- Providing EVV system training and technical support
Refer to 5000 EVV Proprietary System for more information.
2500 Program Provider
Revision 22-4; Effective Sept. 1, 2022
A program provider is an entity that contracts with HHSC or an MCO to provide an EVV service.
Program provider responsibilities include, but are not limited to:
- Following all EVV requirements described in:
- The EVV Policy Handbook
- Texas Administrative Code, Title 1, Part 15, Chapter 354, Subchapter O
- Adhering to policies and requirements of their Medicaid program
- Meeting other applicable HHSC and MCO requirements
- Completing all required EVV training
- Using the EVV system
- Training service providers on the use of EVV
- Ensuring service providers use the EVV system to clock in at the beginning of service delivery and clock out at the end of service delivery
- Managing program provider, service provider and member data within the EVV system
2600 Financial Management Services Agency
Revision 22-4; Effective Sept. 1, 2022
A financial management services agency (FMSA) is an entity that contracts with HHSC or an MCO to provide financial management services to a CDS employer.
FMSA responsibilities include, but are not limited to:
- Following all EVV requirements described in:
- The EVV Policy Handbook
- Texas Administrative Code, Title 1, Part 15, Chapter 354, Subchapter O
- Adhering to policies and requirements of their Medicaid program
- Meeting other applicable HHSC and MCO requirements
- Selecting an EVV system
- Assisting the CDS employer with completing and updating Form 1722, Employer’s Selection for EVV Responsibilities, and entering selections into the EVV system
- Completing all required EVV training
- Using the EVV system
- Managing FMSA, CDS employers, member and service provider data within the EVV system
Refer to 16010 CDS Option Stakeholders for more information.
2700 Member
Revision 22-4; Effective Sept. 1, 2022
A member is a person eligible to receive Medicaid services requiring the use of EVV.
Member responsibilities include, but are not limited to:
- Reviewing and signing Form 1718, Responsibilities and Additional Information, if receiving EVV services through managed care
- Reviewing and signing program specific documentation describing a member’s rights and responsibilities if receiving EVV services administered by the state
- Notifying the program provider if a service provider asks the member to clock in or clock out of the EVV system
2800 CDS Employer
Revision 22-4; Effective Sept. 1, 2022
A CDS employer is a member or legally authorized representative (LAR) who participates in the CDS option.
CDS employer responsibilities include, but are not limited to:
- Completing all required EVV training
- Training their CDS employees on the use of the EVV system
- Ensuring CDS employees use the EVV system to clock in when services begin and clock out when services end
- Approving time worked
- Signing up for GovDelivery to receive the most current news and alerts related to EVV
Refer to 16000 CDS Employer Policies for more information.
3000, Programs and Services Required to Use EVV
Revision 22-4; Effective Sept. 1, 2022
Programs and services required to use EVV are defined in HHSC Texas Administrative Code Section 354.4005, Applicability.
A summary of the personal care services required to use EVV is available on the HHSC EVV webpage.
3100 EVV Service Bill Codes
Revision 21-1; Effective Nov. 1, 2021
The EVV Service Bill Codes Table provides current billing codes for EVV-relevant services in long-term care, acute care and managed care programs.
Program providers and FMSAs must use the appropriate Healthcare Common Procedure Coding System (HCPCS) and modifier combinations in the EVV Services Bill Codes table to prevent EVV visit transaction rejections and EVV claim match denials.
4000, EVV System and Setup
Revision 22-4; Effective Sept. 1, 2022
Program providers and FMSAs must implement and begin using an EVV system before submitting an EVV claim for reimbursement.
Program providers and FMSAs must complete the following steps before using an EVV system.
Step 1: Select an EVV system (Refer to 4100 EVV System Selection)
- EVV vendor system
- EVV proprietary system
Step 2: Complete all EVV trainings (Refer to 4200 EVV Training):
- EVV System
- EVV Policy
- EVV Portal
Step 3: Complete EVV system Onboarding
- Manually enter or electronically import identification data (Refer to 4400 Data Collection)
- Enter or confirm member service authorizations (Refer to 4500 Service Authorizations)
- Setup member schedules (if required) (Refer to 4600 Schedules)
- Create service provider or CDS employee profiles and credentials. (Refer to 4300 Credentialing and 16020 CDS Employer Steps Prior to Using an EVV System)
- For FMSAs only, create CDS employer profiles and credentials depending on the option selected on Form 1722, Employer’s Selection for EVV Responsibilities (Refer to 16020 CDS Employer Steps Prior to Using an EVV System)

4100 EVV System Selection
Revision 21-1; Effective November 1, 2021
State and federal law require program providers and FMSAs to use an EVV system for Medicaid services required to use EVV.
Program Providers and FMSAs must complete the following:
- Select a single EVV system
- Complete the EVV system training, EVV policy training and EVV Portal Trainings
- Complete the EVV system onboarding process
- Begin using the EVV system
Failure to use an EVV system to verify and document the occurrence of a service visit will result in the denial or recoupment of EVV claims by HHSC and MCOs.
Subcontracted providers must use the EVV system selected by the program provider directly contracted with HHSC or an MCO. CDS employers must use the EVV system selected by their FMSA.
There are two types of EVV systems:
- EVV vendor systems from the state vendor pool
- EVV proprietary systems purchased or developed by a program provider or FMSA
4110 EVV Vendor Systems
Revision 22-4; Effective Sept. 1, 2022
An EVV vendor system is an EVV system provided by an EVV vendor in the state vendor pool.
An EVV vendor system is provided at no cost to program providers, FMSAs or CDS employers. Program providers or FMSAs may select one of the following EVV vendor systems available from the state vendor pool.
State Vendor Pool
| EVV Vendor | EVV Vendor System Name | EVV Vendor Contact Information |
|---|---|---|
| DataLogic Software, Inc. | Vesta EVV | Website: vestaevv.com/ Phone: 844-880-2400 |
| First Data Government Solutions | AuthentiCare EVV | Website: solutions.fiserv.com/authenticare-tx Phone: 877-829-2002 |
4120 EVV Proprietary Systems
Revision 22-4; Effective Sept. 1, 2022
An EVV proprietary system is an HHSC-approved EVV system that a program provider or FMSA may use instead of an EVV vendor system that:
- Is purchased or developed by a program provider or an FMSA
- Is used to exchange EVV data with the EVV Aggregator
- Complies with HHSC EVV Policy as it relates to EVV Proprietary Systems
- Complies with HHSC EVV Business Rules for Proprietary Systems
- Complies with the requirements of Texas Government Code Section 531.024172 or its successors
Refer to 2400 EVV Proprietary System Operator and 5000 EVV Proprietary System for more information.
4130 Select an EVV System
Revision 22-4; Effective Sept. 1, 2022
EVV Vendor System Selection
To select an EVV vendor system, program providers or FMSAs must complete, sign, date and submit the EVV Provider Onboarding Form directly to the selected EVV vendor. The EVV Provider Onboarding Form must be signed by the program provider or FMSA signature authority.
EVV vendors may offer software for a fee such as billing solutions. HHSC does not require program providers or FMSAs to buy software when selecting to use an EVV vendor system.
HHSC encourages program providers and FMSAs to research all EVV vendors and their business practices such as clock in and clock out methods, visit maintenance processes and training options before selecting one.
Program providers or FMSAs may visit the TMHP EVV Vendors webpage to learn more about EVV vendor systems.
EVV Proprietary System Selection
Program providers or FMSAs interested in using an EVV proprietary system, must visit the TMHP Proprietary System webpage to review the EVV PSO Onboarding Process and HHSC EVV Proprietary System Approval Process.
To begin the approval process, a program provider or FMSA must submit an EVV Proprietary System Request Form directly to TMHP. The EVV Proprietary System Request Form must be signed by the program provider, FMSA or signature authority.
PSOs must receive written approval from HHSC prior to using an EVV proprietary system.
Contact TMHP at EVV@tmhp.com for questions regarding EVV system selection.
EVV System Administrator
Program providers or FMSAs must appoint an EVV system administrator. The EVV system administrator will administer EVV system access for staff and ensure that the program provider or FMSA enters all necessary data into the EVV system.
Access for staff may include subcontracted or third party personnel, as necessary, to complete visit maintenance tasks. The EVV system administrator must ensure staff who use the EVV system follow HIPAA laws and appropriate security protocols.
4200 EVV Training
Revision 22-4; Effective Sept. 1, 2022
The HHSC EVV Training Policy requires program providers, FMSAs and CDS employers or any staff who performs EVV system operations to complete all required EVV training:
- Prior to using either an EVV vendor system or an EVV proprietary system; and
- Yearly thereafter.
If a program provider or FMSA does not take the following EVV training, it may result in the payer taking enforcement action:
- EVV System
- EVV Policy
- EVV Portal
If a program provider does not provide Clock In and Clock Out Methods training to their service providers, it may result in the payer taking enforcement action.
If a CDS employer does not take EVV system and EVV policy trainings or provide training to their CDS employee(s) as applicable, the following may result:
- CDS employee(s) may experience a delay in payment or inaccurate payments if the EVV system is not used correctly.
- An FMSA or payer may require the CDS employer to complete a corrective action plan (CAP).
CDS employers must take EVV system and EVV policy trainings to:
- Gain a basic understanding of EVV requirements.
- Train CDS employees on the approved clock in and clock out methods.
The EVV vendor or PSO will not grant access to the EVV system until the program provider, FMSA or CDS employer has completed EVV system training.
The payers may request proof of completed trainings. Do not submit proof of training completion to HHSC, an MCO or TMHP unless requested.
Proof of completed trainings must include the:
- Name of the training
- Name of the person completing the training
- Date of the training
Program providers, FMSAs and CDS employers can review the EVV Training Requirements Checklists found on the EVV webpage for more information.
The EVV vendor, HHSC, MCOs and TMHP may offer EVV trainings in different delivery methods, such as but not limited to:
- Computer-based training (CBT)
- Instructor-led training (ILT)
- Webinars
Contact your EVV vendor, HHSC, MCO or TMHP for details on specific training delivery methods.
4210 EVV Training Requirements for Program Providers
Revision 21-1; Effective Nov. 1, 2021
Program providers must complete the required EVV training shown in the table below.
EVV system users are staff who have access to the EVV system, perform EVV system operations and visit maintenance in the EVV vendor system or EVV proprietary system. EVV portal users are staff who have access to the EVV portal, conduct visit or claim searches and generate reports. Billing staff are staff who submit Medicaid claims for an EVV-required service.
Program Providers
| EVV Training Requirement | Taken By | Provided By |
|---|---|---|
| EVV System Training | EVV system users | EVV vendor or EVV PSO |
| EVV Portal Training |
| TMHP |
| EVV Policy Training |
| Payer (HHSC or MCO) |
Program providers must keep up-to-date training records for their staff.
Program providers who have received written approval from HHSC to use an EVV proprietary system must train all users on the proper use of the EVV proprietary system, to include clock in and clock out methods.
4220 EVV Training Requirements for FMSAs
Revision 22-2; Effective March 1, 2022
FMSA staff must complete the required EVV training shown in the table below.
EVV system users are staff who have access to the EVV system, perform EVV system operations and complete visit maintenance in the EVV vendor system or EVV proprietary system. EVV Portal users are staff who have access to the EVV Portal, conduct visit or claim searches and generate reports. Billing staff are staff who submit Medicaid claims for an EVV-required service.
FMSAs
| EVV Training Requirement | Taken By | Provided By |
|---|---|---|
| EVV System Training |
| EVV vendor or EVV PSO |
| EVV Portal Training |
| TMHP |
| EVV Policy Training |
| Payer (HHSC or MCO) |
FMSAs must keep up-to-date training records for their staff. FMSAs may request training records from their CDS employers.
4230 EVV Training Requirements for CDS Employers
Revision 22-2; Effective March 1, 2022
CDS employers complete applicable required EVV training. If the CDS employer has a designated representative (DR), the DR completes the required EVV training based on the option selected by the CDS employer. This information is shown in the table below.
CDS employers must train their CDS employees on the clock in and clock out methods with assistance from the EVV vendor or the EVV PSO.
See details in table below for:
- CDS employer training based on delegation of visit maintenance on Form 1722, CDS Employer's Selection for Electronic Visit Verification Responsibilities.
- If a CDS employer switches their option by completing a new Form 1722, CDS Employer's Selection for Electronic Visit Verification Responsibilities, they must take the proper training for that option, before being granted greater access to the EVV system by an EVV vendor, their FMSA or an EVV PSO.
Note: HHSC policy training is available in Spanish or English.
If the CDS employer selected:
| Form 1722 Options | EVV Training Requirement | Provided By |
|---|---|---|
| Option 1: The CDS employer agrees to complete all visit maintenance and approve their employee's time worked in the EVV system. |
| EVV vendor or EVV PSO (FMSA) |
| Payer (HHSC or MCO) or FMSA | |
| Option 2: The CDS employer elects to have their FMSA complete all visit maintenance on their behalf. However, the CDS employer will approve their employee's time worked in the EVV system. |
| EVV vendor or EVV PSO (FMSA) |
| Payer (HHSC or MCO) or FMSA | |
| Option 3: The CDS employer elects to have their FMSA complete all visit maintenance on their behalf. The FMSA will confirm the employee's time worked in the EVV system based on approval documentation from the CDS employer. |
| EVV vendor or EVV PSO (FMSA) |
| Payer (HHSC or MCO) or FMSA |
The CDS employer must keep up-to-date training records of their training completions and provide training records to their FMSA, HHSC or their MCO, if requested.
Note: EVV policy trainings may vary if your payer is an MCO. Please check with your MCO if you have questions on EVV policy trainings and requirements.
4240 Training Requirements for Service Providers and CDS Employees
Revision 22-2; Effective March 1, 2022
Service providers and CDS employees must complete the required EVV training shown in the table below.
The EVV vendor or EVV PSO will provide materials and resources.
Service Providers and CDS Employees:
| EVV Training Requirement | Provided By |
|---|---|
| Clock In and Clock Out Methods | Program Provider or CDS Employer |
The CDS employer must keep up-to-date training records of service provider and CDS employee training completions by using Form 1732, Management and Training of Service Provider. Form 1732 should be provided to the FMSA.
4250 EVV Training Registration
Revision 21-1; Effective Nov. 1, 2021
To register for EVV training:
- EVV System: Visit your EVV vendor website or contact your EVV PSO (FMSA).
- EVV Policy: Visit the HHSC or MCO EVV webpage.
- Access the HHSC Learning Portal then create an account.
- EVV Portal Training: Visit the TMHP website
- Access the TMHP Learning Management System (LMS) and create an account.
For questions related to training, contact:
| Topic | Contact |
|---|---|
| EVV Policy |
|
| EVV Portal |
|
| EVV vendor or EVV PSO System |
|
4300 Credentialing
Revision 21-1; Effective Nov. 1, 2021
The FMSA is responsible for creating credentials (username and temporary password) for the CDS employer and the CDS employee.
For the CDS Employer
The credentials will be sent by the EVV system or the FMSA to the CDS employer based on the email account the FMSA entered in the EVV system. If a member is not the CDS employer, the FMSA will include the CDS employer's name in the member profile and provide credentials to the CDS employer. If the member also has a DR, both the CDS employer and the DR will have their own unique credentials.
The CDS employer uses the credentials to log in to the EVV system. After the CDS employer logs in to the EVV system, the temporary password can be changed, and a new unique password can be created.
The FMSA can only see the CDS employer's username and email address in the EVV system. However, both the FMSA and the CDS employer can change the password.
There are two common reasons why a CDS employer has not received their credentials, and therefore must contact their FMSA.
- The FMSA has not created credentials for the CDS employer
- The information entered by the FMSA was incorrect
- The FMSA can correct the email address and resend credentials to the CDS employer
For the CDS Employee
The FMSA or the CDS employer provides the credentials to the CDS employee.
Contact your EVV vendor to determine if the FMSA or the CDS employer will provide the CDS employee credentials.
Program Providers
The program provider is responsible for creating credentials such as username and temporary password, for all program provider staff including service providers.
4400 Data Collection
Revision 22-2; Effective March 1, 2022
In alignment with Texas Government Code Section 531.024172 and federal requirements, the EVV system must allow for verification of the following critical data elements relating to the delivery of Medicaid services:
- Type of service provided
- Name of the recipient who had the service
- Date and times the provider began and ended the service delivery visit
- Location, including the address and geolocation, where the service was provided
- Name of the person who provided the service
- Other information the commission determines is necessary to ensure the accurate adjudication of Medicaid claims
HHSC categorizes critical data elements as:
- Identification data
- Visit data
Identification Data
Before using the EVV system, the program provider or FMSA must enter or import the following identification data into the EVV system:
- Type of service provided (service authorization data).
- Name of the recipient who had the service (member data).
- Name of the person who provided the service (service provider data).
- Other information HHSC determines is necessary to ensure the accurate adjudication of Medicaid claims (program provider, FMSA or CDS employer information).
Program providers and FMSAs must manually enter or electronically import identification data during the EVV system onboarding process, or after the onboarding process for new members.
Once the program provider or FMSA has completed the entry of all identification data, the service provider or CDS employee may begin to use the EVV system.
Program providers and FMSAs must maintain the identification data as needed.
The program provider or FMSA is solely responsible for maintaining accurate and up-to-date data within the EVV system. This includes information managed or maintained by a third party or subcontractor. If the program provider or FMSA identifies data errors, they must act to resolve the inaccuracy.
Visit Data
When the service provider clocks in and clocks out of the EVV system, the system captures the following visit data:
- Type of service provided (service authorization data).
- Name of the recipient who had the service (member data).
- Date and times the provider began and ended the service delivery visit.
- Location, including the address and geolocation, where the service was provided.
- Name of the person who provided the service (service provider data).
Missing or incorrect identification data and visit data in the EVV system results in:
- Rejected EVV visit transactions
- Denied or recouped EVV claims
- Inaccurate EVV standard reports
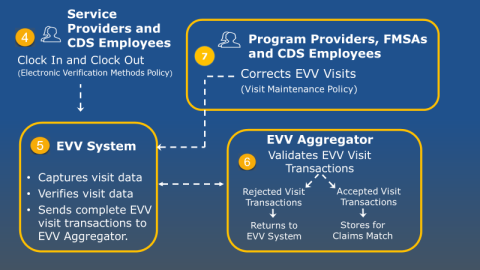
4410 Data Collection Overview Diagram
Revision 21-1; Effective Nov. 1, 2021
The EVV system:
- Electronically captures and verifies critical data elements to confirm service delivery.
- Validates identification data against data received from the Texas Medicaid system.
- Sends a complete, accurate and validated EVV visit transaction to the EVV Aggregator for use in the EVV claims matching process.

Contact your payer for questions about the data elements.
Contact your EVV vendor or EVV PSO for questions about entering data into the EVV system.
4500 Service Authorizations
Revision 22-4; Effective Sept. 1, 2022
Payers must authorize and document services a member is eligible to receive.
Program providers or FMSAs may receive authorization for member services through one of the following, depending on the Medicaid program:
- Service authorization
- Prior authorization
- Individual plan of care (IPC)
- Individual service plan (ISP)
- Community care service notification
The EVV system refers to authorization from a payer as service authorization.
Service authorizations, when entered into the EVV system, must include at least the following when applicable:
- Payer
- Provider (National Provider Identifier (NPI), Atypical Provider Identifier (API), Texas Identification Number (TIN))
- Member Medicaid ID
- Service group, service code or HCPCS and Modifier
- Authorization start date and end date
The EVV system will electronically retrieve the most recent service authorization from TMHP for the following HHSC programs:
- Community Living Assistance and Support Services (CLASS) Waiver
- Deaf Blind Multiple Disabilities (DBMD) Waiver
- Home and Community-based Services (HCS) Waiver
- Texas Home Living (TxHmL) Waiver
- Personal Care Services (PCS)
- Primary Home Care (PHC)
- Family Care (FC)
- Community Attendant Services (CAS)
- Youth Empowerment Service (YES) Waiver
Program providers and FMSAs must manually enter service authorizations into the EVV system for the following HHSC and managed care programs:
- Home and Community-based Services - Adult Mental Health (HCBS-AMH)
- STAR Health
- STAR Kids
- STAR+PLUS
- STAR+PLUS Home and Community Based Services (HCBS)
- STAR+PLUS Medicare-Medicaid Plan (MMP)
Failure to enter the most current service authorization issued by the payer into the EVV system may result in the need for visit maintenance or the payer may deny or recoup related EVV claims. Program providers or FMSAs may manually enter service authorization changes and updates into the EVV system at any time.
Program providers and FMSAs must confirm all electronically received service authorizations in the EVV system to ensure eligibility for each member.
Contact your payer with questions about service authorization requirements. Contact your EVV vendor or PSO with questions on the entry of service authorizations into the EVV system.
4600 Schedules
Revision 22-3; Effective June 1, 2022
A schedule is planned frequency and duration of an EVV service entered in to the EVV system.
EVV policy does not require program providers and FMSAs to enter schedules in to the EVV system. Service delivery can occur with or without a schedule.
Program providers and FMSAs must follow their program requirements for schedules to determine if they are required to enter a schedule in to the EVV system. Failure to follow program requirements may result in EVV claims being recouped.
Only EVV users with appropriate security access can enter a schedule in to the EVV system. A complete service provider or CDS employee profile must exist in the EVV system prior to a program provider or FMSA entering a schedule in to the EVV system. CDS employers cannot enter schedules in to the EVV vendor systems.
The program provider or FMSA is responsible for monitoring service authorizations to ensure a schedule entered in to the EVV system has enough units available for service delivery. Refer to 4500 Service Authorizations for more information.
An EVV visit transaction that matches against a schedule will auto-verify if there are no exceptions or critical errors. EVV visit transactions that do not match against a schedule or have exceptions or critical errors will require visit maintenance.
If the EVV system finds exceptions or critical errors visit maintenance is required and the program provider, FMSA or CDS employer must:
- Select the most appropriate EVV reason code. Refer to 9000 EVV Reason Code for more information.
- Document the reason for working outside of the schedule either in the free text using the EVV system or as required by program requirements.
Refer to 6000 EVV Visit Transaction and 8000 Visit Maintenance for more information.
Contact your program representative with questions about schedule requirements.
No Schedule
If a program provider or FMSA does not choose a schedule type in the EVV system, the default is no schedule.
Service providers and CDS employees can still clock in and clock out of the EVV system if the program provider or FMSA does not choose a schedule type.
An EVV visit transaction will match without a schedule if there are no exceptions or critical errors.
EVV Vendor Systems
EVV vendor systems from the state vendor pool allow the program provider and FMSA to select from three different schedule types when entering schedules in to the EVV system:
- Daily Fixed
- Daily Variable
- Weekly Variable
A member can have one schedule type for one service and another schedule type or no schedule type for another service. Only one schedule type can be selected for a specific member’s service at a time.
The EVV vendor system will alert the program provider or FMSA when:
- The service provider or CDS employee on the schedule does not have a complete profile in the EVV system
- A schedule is entered without a service authorization
- A schedule does not match an existing service authorization
- An updated service authorization is available in the EVV system
- A change to the schedule type is made
Contact your EVV vendor to learn about schedule types and auto-verification of EVV visit transactions.
Visit Maintenance Reduction Features
Visit maintenance reduction features are available in the EVV vendor systems for program providers and FMSAs who enter Daily Fixed or Daily Variable schedule types in the EVV system. Visit maintenance reduction features help to reduce visit maintenance.
Available visit maintenance reduction features in the EVV vendor systems are:
- Optional Expanded Time for Auto-Verification
- Optional Automatic Downward Adjustment
Refer to 8100 Visit Maintenance Reduction Features for more information.
EVV Proprietary Systems
HHSC does not require a PSO to offer schedule types in their EVV proprietary system. The EVV PSO may choose to implement an alternate schedule type or follow EVV policy for Daily Fixed, Daily Variable or Weekly Variable schedule types.
Contact your EVV PSO to learn about schedule types.
4610 Schedule Types
Revision Notice 22-3; Effective June 1, 2022
Daily Fixed Schedule
The Daily Fixed Schedule type is selected when service delivery must follow the member’s plan of care exactly.
A program provider or FMSA can select this schedule type if program requires the service provider deliver EVV services in accordance with the member’s plan of care.
Program providers or FMSAs have the option to turn on or off visit maintenance reduction features as needed for each member and service in the EVV system.
Schedule Match Criteria – Daily Fixed Schedule
| Schedule Type | Schedule Match Criteria |
|---|---|
| Daily Fixed Schedule | Visit:
|
| Daily Fixed Schedule with Optional Expanded Time for Auto-Verification | Visit:
|
| Daily Fixed Schedule with Optional Expanded Time for Auto-Verification and Optional Automatic Downward Adjustment |
|
Daily Variable Schedule
The Daily Variable Schedule type is selected when service delivery allows for flexibility when scheduling EVV services based on the member’s plan of care.
A program provider or FMSA can select this schedule type if program requirements allow flexible service delivery within a day based on the schedule entered in the EVV system.
Program providers or FMSAs have the option to turn on or off visit maintenance reduction features as needed for each member and service in the EVV system.
Schedule Match Criteria – Daily Variable Schedule
| Schedule Type | Schedule Match Criteria |
|---|---|
| Daily Variable Schedule | Visit:
|
| Daily Variable Schedule with Optional Expanded Time for Auto-Verification | Visit:
|
| Daily Variable Schedule with Optional Expanded Time for Auto-Verification and Optional Automatic Downward Adjustment |
|
Weekly Variable Schedule
The Weekly Variable Schedule type is selected when the member’s plan of care allows for maximum flexibility in service delivery.
The program provider or FMSA can select this schedule type if program requirements allow service delivery throughout the week based on the needs and schedule of the member rather than the schedule entered in to the EVV system.
All visit maintenance reduction features are turned off and cannot be turned on for this schedule type.
Schedule Match Criteria- Weekly Variable Schedule
| Schedule Type | Schedule Match Criteria |
|---|---|
| Weekly Variable Schedule |
|
4700 EVV System Transfer
Revision 22-4; Effective Sept. 1, 2022
A program provider or FMSA may complete the following system transfer types:
- EVV vendor system to another EVV vendor system.
- EVV vendor system to an EVV proprietary system.
- EVV proprietary system to an EVV vendor system.
- EVV proprietary system to another EVV proprietary system.
Program providers and FMSAs who have not selected an EVV system must follow 4100 EVV System Selection.
During a system transfer, the program provider and FMSA must:
- Use their current EVV system until they have successfully transferred to the new EVV system.
- Document all EVV visits for dates of service:
- Before the Go-Live date in the current EVV system.
- On or after the Go-Live date in the new EVV system.
The Go-Live date is the date the program provider or FMSA begins using a new EVV system.
Program providers, FMSAs and CDS employers must complete visit maintenance in the same EVV system in which the EVV visit transaction was created within the visit maintenance time frame.
Program providers and FMSAs must:
- Not collect visit data in more than one EVV system at a time.
- Transition all visit data collection to the new EVV system as of the Go-Live date.
- Return all alternative devices supplied by the current EVV vendor, after the Go-Live date with the new EVV system in accordance with the requirements of the EVV vendor.
Data Transfer Requirements
The program provider or FMSA may, but is not required to, transfer data from the current EVV system to the new EVV system. The EVV Data Transfer Guide is available on the TMHP EVV Proprietary Systems webpage and provides standardized templates for data transfer. The data transfer requirements by transfer type are provided below.
- EVV vendor system to another EVV vendor system: The program provider or FMSA must notify the current EVV vendor which data elements they want to have imported into the new EVV vendor system, if any. The EVV vendors are responsible for the data transfer process.
- EVV vendor system to an EVV proprietary system: The program provider or FMSA must notify the current EVV vendor which data elements they want exported from the EVV vendor system, if any. The EVV vendor will provide data elements in the format defined in the EVV Data Transfer Guide. The program provider or FMSA is responsible for importing the data into the EVV proprietary system.
- EVV proprietary system to an EVV vendor system: If the program provider or FMSA wants data imported into the EVV vendor system, they must provide data elements to the EVV vendor in the format defined in the EVV Data Transfer Guide. The EVV vendor is responsible for importing the data into the EVV vendor system.
- EVV proprietary system to another EVV proprietary system: The program provider or FMSA can use the format defined in the EVV Data Transfer Guide or a custom format to transfer data elements between EVV proprietary systems, if needed. The program provider or FMSA is responsible for the data transfer process.
4710 How to Transfer to an EVV Vendor System
Revision 22-4; Effective Sept. 1, 2022
Program providers and FMSAs who wish to transfer from an EVV vendor system to another EVV vendor system must request a transfer at least 120 days before the desired Go-Live date. The transfer may occur before the 120 days if program provider or FMSA and EVV vendors agree on an earlier date.
The 120-day transfer time frame allows for:
- Training on the new EVV system.
- Transfer of data, if requested by the program provider or FMSA.
- Completion of all tasks necessary to begin using the new EVV system.
FMSAs must notify CDS employers 60 days in advance of the planned Go-Live date to allow time for retraining CDS employers and their CDS employees on the new EVV system.
Program providers or FMSAs must:
- Complete a Termination Form with their current EVV vendor 120 days before the desired Go-Live date.
- Complete an EVV Provider Onboarding Form with the new EVV vendor 120 days before the desired Go-Live date:
- Select “transfer” on the form
- Submit to the new EVV vendor
Vendor Transfer Process:
- New EVV vendor will contact the signature authority or the EVV System Administrator within five business days of receipt to confirm the request to transfer and acknowledge receipt.
- Current EVV vendor will contact the program provider or FMSA to discuss the transfer request and agree upon a date to transfer data to the new EVV vendor.
- Current EVV vendor will communicate the date to transfer data to the new EVV vendor and TMHP.
- New EVV vendor must import data within five business days of receipt on behalf of the program provider and FMSA.
- New EVV vendor will notify the program provider or FMSA and TMHP within five business days of completing the data transfer.
- New EVV vendor will provide further onboarding and EVV system training instructions.
Program providers or FMSAs transferring to an EVV vendor system:
- Must follow 4100 EVV System Selection and 4700 EVV System Transfer.
- Must complete EVV system training before using the new EVV system.
- Will not receive a grace period for complying with EVV Policy.
- May have EVV claims denied or recouped if there are no accepted EVV visit transactions.
Contact the selected EVV vendor or email TMHP for questions about EVV system transfer.
4720 How to Transfer to an EVV Proprietary System
Revision 22-4; Effective Sept. 1, 2022
If transferring to an EVV proprietary system from an EVV vendor system, a program provider or FMSA must submit:
- An EVV Proprietary System Request Form directly to TMHP.
- A Termination Form to the current EVV vendor within seven days of HHSC accepting the program provider or FMSA into an ORR session.
If transferring to an EVV proprietary system from another EVV proprietary system, the PSO must submit an EVV Proprietary System Request Form directly to TMHP.
Transferring to an EVV proprietary system can only occur after:
- Successful completion of the PSO Onboarding Process.
- HHSC provides written approval of the EVV proprietary system.
- HHSC and the PSO agree upon on a Go-Live date.
Program providers or FMSAs who transfer to an EVV proprietary system:
- Must provide training on the EVV proprietary system.
- Must complete EVV system training before using the EVV proprietary system. Refer to 5000 EVV Proprietary System for more information.
- Will not receive a grace period for complying with EVV Policy.
- May have EVV claims denied or recouped if there are no accepted EVV visit transactions.
Contact the selected EVV vendor or email TMHP for questions about the EVV system transfer.
5000, EVV Proprietary System
Revision 22-4; Effective Sept. 1, 2022
Section 531.024172 of the Texas Government Code provides the authority for HHSC to recognize an EVV proprietary system as complying with EVV standards and policy requirements. Program providers or FMSAs approved by HHSC to operate an EVV proprietary system must comply fully with the EVV Policy Handbook.
An EVV proprietary system is an HHSC-approved EVV system that a program provider or FMSA may use instead of an EVV vendor system that:
- Is purchased or developed by a program provider or an FMSA.
- Is used to exchange EVV data with the EVV Aggregator.
- Complies with HHSC EVV Policy as it relates to EVV Proprietary Systems.
- Complies with HHSC EVV Business Rules for Proprietary Systems.
- Complies with the requirements of Texas Government Code Section 531.024172 or its successors.
Program providers or FMSAs must submit an EVV Proprietary System Request Form directly to TMHP to enter the PSO Onboarding Process.
There are two onboarding paths a program provider or FMSA can choose:
- The Standard Path is for requesting approval to use an EVV system that has not been previously approved by HHSC.
- The Expedited Path is for requesting approval to use an existing operational EVV system that HHSC has previously approved. The list of approved EVV Proprietary Systems is on the TMHP EVV Proprietary Systems webpage.
View the PSO Onboarding Process guide on the TMHP EVV Proprietary Systems webpage for more information about each Path.
Program providers or FMSAs must meet applicable HHSC EVV Business Rules for Proprietary Systems posted on the TMHP Proprietary Systems webpage and follow all HHSC EVV standards and policy requirements. These include, but are not limited to:
- State and federal laws governing EVV
- HHSC EVV Policy Handbook
- HHSC EVV Business Rules for Proprietary Systems
- PSO Onboarding Process
After the program provider or FMSA has received HHSC approval to use an EVV proprietary system, they are known as a PSO. Refer to 2400 EVV Proprietary System Operator for more information.
The PSO must:
- Follow all requirements specified through HHSC or MCO program provider or FMSA contracts.
- The PSO will be subject to HHSC and MCO EVV Compliance Reviews and other compliance monitoring under the program provider or FMSA contract(s). Refer to 5080 Proprietary System Operator Compliance for more information.
- Inform HHSC if the EVV proprietary system is not compliant with EVV standards and requirements or when making significant changes to the EVV system.
- Notify the payers when transferring from an EVV proprietary system and when status changes occur.
The PSO may be subject to periodic verification, system testing and auditing as specified by HHSC.
PSOs, EVV proprietary system vendors and outside entities may only use the HHS logo on materials and websites if approved by the HHSC Office of Communications.
5010 Reimbursement for Use of an EVV Proprietary System
Revision 22-4; Effective Sept. 1, 2022
HHSC does not directly reimburse program providers and FMSAs for the use of an EVV proprietary system. However, program providers and FMSAs can report costs related to their EVV proprietary system through established Medicaid cost reporting processes.
HHSC evaluates this data when setting future Medicaid rates. Not all Medicaid programs utilize cost reports.
Contact the HHSC Provider Finance Department at ProviderFinanceDept@hhs.texas.gov or contact your MCO for more information about Medicaid cost reporting.
5020 EVV Proprietary System Operator Responsibilities
Revision 22-4; Effective Sept. 1, 2022
The PSO is required to meet Texas Government Code Section 531.024172 and HHSC EVV Business Rules for Proprietary Systems governing the use of EVV proprietary systems.
A PSO:
- Must comply with the Health Insurance Portability and Accountability Act (HIPAA) and the American Disabilities Act (ADA).
- Agrees to forego use of a cost free EVV system provided by the state.
- Assumes responsibility for the design, development, operation and performance of the EVV proprietary system.
- Assumes responsibility for all costs to develop, implement, operate and maintain the EVV proprietary system.
- Is responsible for the accuracy of EVV data collected, stored and reported by the EVV proprietary system.
- Submits EVV visit transactions to the EVV Aggregator.
- Is responsible for ensuring EVV visit transactions from the EVV proprietary system are accepted by the EVV Aggregator.
- Assumes liability and risk for the use of the EVV proprietary system.
- Must maintain all system data, backup data and historical data to comply with and support all legal, regulatory and general business purposes.
- Must train EVV proprietary system users, including state and MCO staff.
- Must provide system access to state staff, TMHP staff, MCO staff (if applicable) and other state and federal entities as required.
- Must provide HHSC-approved clock in and clock out methods associated with the EVV proprietary system at no cost to the program provider, FMSA, CDS employer, service provider, member, HHSC, MCO or TMHP.
- Assumes responsibility for the functionality and accuracy of all clock in and clock out methods distributed to service providers and CDS employees.
- Must ensure use of the EVV proprietary system will not conflict with:
- EVV Member Responsibilities and Additional Information
- EVV policies or requirements
- HHSC EVV Business Rules for Proprietary Systems
- Texas Government Code Section 531.024172
5030 EVV Proprietary System Onboarding Process
Revision 22-4; Effective Sept. 1, 2022
To begin the proprietary system onboarding process, a program provider or FMSA must follow the PSO Onboarding Process posted on the TMHP Proprietary Systems webpage and submit an EVV Proprietary System Request Form directly to TMHP. The EVV Proprietary System Request From must be signed by a signature authority for the program provider or FMSA.
After submission of the EVV Proprietary System Request Form, HHSC, TMHP and the program provider or FMSA will meet to review the detailed requirements for the PSO Onboarding Process and the major milestones associated with the assigned ORR session.
The program provider or FMSA must notify HHSC if the agreed project timeline associated with the ORR session has any conflicts. If HHSC, TMHP and the program provider or FMSA determine the timeline is at risk, HHSC may require the program provider or FMSA to use an EVV vendor system until HHSC approves the EVV proprietary system for use.
Program providers or FMSAs may use their EVV proprietary system for one or more NPI/API or TIN combinations when onboarding if the program provider or FMSA intends to use the same EVV proprietary system for each NPI/API or TIN combination.
Key Personnel
The program provider or FMSA must identify the following key personnel for proprietary system administration:
- Onboarding Project Manager
- Manages the PSO Onboarding Process for the program provider or FMSA.
- Acts as the program provider or FMSA’s primary point of contact during the PSO Onboarding Process.
- Provides progress updates and escalates issues that may arise to TMHP and HHSC during the PSO Onboarding Process.
- May be a program provider or FMSA representative or a proprietary system software vendor representative.
- EVV System Administrator (Refer to 1600 Key Terms for more information)
- Manages EVV system access.
- Acts as the PSO’s primary point of contact after the Go-Live date.
- Is listed on the EVV Proprietary System Access and Training Guide on the HHSC EVV Proprietary Systems webpage.
- May be a program provider or FMSA representative or a proprietary system software vendor representative.
- EVV Training Contact
- Is responsible for providing EVV system training.
- Is listed on the EVV Proprietary System Access and Training Guide on the HHSC EVV Proprietary Systems webpage.
- May be a program provider or FMSA representative or a proprietary system software vendor representative.
- Signature Authority (Refer to 1600 Key Terms for more information)
- Must have legal authority to sign contracts and make transactional decisions for the program provider or FMSA.
- Is responsible for:
- Signing the EVV Proprietary System Request Form.
- Certifying compliance with the HHSC EVV Business Rules for Proprietary Systems and HHSC EVV policies.
- Selecting a Go-Live date for the proprietary system after HHSC approves the system.
- Receiving and responding to HHSC correspondence regarding non-compliance.
Key personnel may be filled by the same person or different people.
Program providers and FMSAs must maintain current key personnel contact information and provide new or updated contact information to HHSC within five business days of any change.
5040 EVV Proprietary System Operational Readiness Review
Revision 22-4; Effective Sept. 1, 2022
HHSC and TMHP conduct a validation process referred to as ORR to determine if a program provider or FMSA is approved to operate an EVV proprietary system.
HHSC reviews requests to enter an ORR session from program providers or FMSAs on a first-come, first-served basis. This is determined by the date of receipt of the EVV Proprietary System Request Form. Program providers or FMSAs that submitted the EVV Proprietary System Request Form and who have not completed the ORR are placed on a waiting list and will receive first choice of these sessions.
HHSC determines the number of program providers or FMSAs taking part in each ORR session.
Program providers or FMSAs must ensure they have a fully developed and compliant EVV system which meets all HHSC requirements by the ORR begin date for their chosen session.
Program providers or FMSAs participating in a Standard Path ORR must demonstrate compliance through four methods:
- Certification – Program providers or FMSAs must certify compliance with Texas Government Code Section 531.024172, HHSC EVV Business Rules for Proprietary Systems and HHSC EVV Policy Handbook.
- Documentation – Program providers or FMSAs must provide specified documentation for HHSC review.
- Demonstration – Program providers or FMSAs must show system functionality using specific HHSC-approved scenarios.
- Trading Partner Testing – Program providers or FMSAs must complete Trading Partner Testing with TMHP according to specific HHSC-approved scenarios.
Program providers or FMSAs participating in an Expedited Path ORR must demonstrate compliance through two methods:
- Certification – Program providers or FMSAs must certify compliance with Texas Government Code Section 531.024172, HHSC EVV Business Rules for Proprietary Systems and HHSC EVV Policy Handbook.
- Trading Partner Testing – Program providers or FMSAs must complete Trading Partner Testing with TMHP according to specific HHSC-approved scenarios.
Program providers or FMSAs must receive a score of 100% for each method to receive HHSC approval.
A program provider or FMSA that does not pass the ORR must continue to use their current EVV system or select an EVV vendor system to comply with HHSC EVV standards and policy requirements.
Refer to 4130 Select an EVV System for more information.
5050 Success or Failure of the Operational Readiness Review
Revision 22-4; Effective Sept. 1, 2022
HHSC determines the success or failure of the EVV proprietary system based on the outcome of the ORR.
If the program provider or FMSA achieve a 100% score for the ORR, TMHP on behalf of HHSC will send an email to the program provider or FMSA:
- Requesting a preferred Go-Live date.
- Asking if they want to be added to the public-facing list of EVV Proprietary Systems approved by HHSC.
The email is followed by a formal letter with HHSC’s approval.
If the program provider or FMSA fails ORR:
- TMHP on behalf of HHSC will send an email notifying the program provider or FMSA of the failure.
- HHSC will send a formal letter listing the failed scenarios, test cases and a list of the HHSC EVV Business Rules for Proprietary Systems that were not validated.
- The program provider or FMSA must either continue with their current EVV system, if applicable, or select and onboard with an EVV vendor system to comply with HHSC EVV standards and policy requirements.
Refer to 4000 EVV System and Setup, 4110 EVV Vendor Systems, 4130 Select an EVV System and 4700 EVV System Transfer for more information.
5060 EVV Proprietary System General Operations
Revision 22-4; Effective Sept. 1, 2022
EVV Proprietary System Training
The PSO is responsible for training all EVV proprietary system users on the proper use of the EVV system including clock in and clock out methods.
Clock In and Clock Out Methods
The PSO must:
- Select one or more clock in and clock out methods from the three HHSC-approved methods described in Section 7000 Clock In and Clock Out Methods.
- Allow manual entry of EVV visit data.
- Successfully demonstrate each selected clock in and clock out method and get written approval from HHSC during the ORR.
- Follow the HHSC EVV Policy Handbook and follow specific HHSC EVV Business Rules for Proprietary Systems related to the selected clock in and clock out method(s).
- HHSC may waive any rules and reports specific to a clock in and clock out method not selected.
The PSO is responsible for the functionality and accuracy of all clock in and clock out methods distributed to service providers and CDS employees.
Any alternative device approved by HHSC must derive the exact clock in and clock out date and time. An alternative device must only be used in the member’s home unless the alternative device has a geo-location capability.
All EVV visits, including those created using the alternative device are subject to the requirements of 8050 Visit Maintenance Time Frames. For example, if the alternative device generates codes, the EVV proprietary system must not allow codes to be entered to create a visit after the visit maintenance time frame.
Refer to 7000 Clock In and Clock Out Methods and 8000 Visit Maintenance for more information.
EVV Proprietary System Maintenance
The PSO:
- Is fully responsible for ongoing maintenance of the EVV proprietary system and must not make changes that conflict with any EVV standards and policy requirements.
- Must inform HHSC within two business days of discovery if the EVV proprietary system is not compliant with any EVV standards and policy requirements.
- Must notify HHSC of any planned system changes that alter an HHSC-approved component of the EVV proprietary system.
- Based on the nature of the change, approval from HHSC may be required before the PSO implements the change.
HHSC may modify EVV standards and policy requirements, including the HHSC EVV Business Rules for Proprietary Systems. HHSC will notify the PSO of any modifications to policy or the HHSC EVV Business Rules for Proprietary Systems. The PSO is responsible for:
- Making updates to the EVV proprietary system to comply with the latest versions of the policies or HHSC EVV Business Rules for Proprietary Systems within the HHSC-approved time frame.
- Certifying compliance with the latest versions of the policies or HHSC EVV Business Rules for Proprietary Systems.
HHSC will provide PSOs a specified time frame to make updates to their EVV proprietary system resulting from modifications to policies, requirements and HHSC EVV Business Rules for Proprietary Systems. Typically, HHSC will provide a minimum of 90 days for PSOs to complete the updates but may provide a different time frame depending on the nature of the change. PSOs may be required to make changes in less than 90 days if HHSC determines that the change is required to address an immediate need.
HHSC will specify ORR steps the PSO must complete before implementation.
TMHP will assist the PSO with resolving production problems in the EVV proprietary system for data exchange with the EVV Aggregator as needed.
5070 Access to the EVV Proprietary System
Revision 22-4; Effective Sept. 1, 2022
All PSOs must:
- Provide immediate, direct, on-site access to state staff and MCOs with which it has a contractual relationship at no cost to the state or MCO.
- Limit MCO access to the MCO’s respective member visit data only, and only for dates of service within the time frame covered by the PSO contract with the MCO.
- This access must be allowed indefinitely after the PSO’s contract with the MCO ends, in accordance with applicable law.
- Provide HHSC, MCOs and proprietary system users access to standard and ad hoc reports and any data necessary to verify EVV usage in accordance with EVV Business Rules for Proprietary Systems.
- Ensure access by the program provider, FMSA, PSO, HHSC and MCOs, if applicable, to historical data which may live in the old EVV system.
Additionally, PSOs that are FMSAs must:
- Provide access for CDS employers who select Option 1 or Option 2 on Form 1722, Employer’s Selection for Electronic Visit Verification Responsibilities, to the EVV proprietary system.
- Provide EVV proprietary system read-only access to CDS employers who select Option 3 on Form 1722, Employer’s Selection for Electronic Visit Verification Responsibilities, if requested.
5080 Proprietary System Operator Compliance
Revision 22-4; Effective Sept. 1, 2022
EVV Compliance Reviews
PSOs are subject to EVV Compliance Reviews.
Payers use EVV data in the EVV Aggregator as the system of record for compliance reviews, specifically the:
- EVV Usage Report
- EVV Reason Code Usage and Free Text Report located in the EVV Portal and EVV system
- EVV Landline Phone Verification Report
Payers may perform other compliance reviews based on data in the EVV proprietary system.
Refer to 10000 EVV Compliance Reviews for more information.
Compliance with HHSC EVV Business Rules for Proprietary Systems and HHSC EVV Policy
If HHSC determines that a PSO is not in compliance with the HHSC EVV Business Rules for Proprietary Systems or HHSC EVV policy, HHSC may:
- Require the PSO to correct the non-compliance within a time frame specified by HHSC.
- Require the EVV Aggregator to reject EVV visit transactions from the proprietary system until HHSC determines the non-compliance is corrected.
- Cancel the use of the EVV proprietary system if the PSO fails to correct the non-compliance within the specified time frame set by HHSC.
- Cancel the use of an EVV proprietary system without giving the PSO the opportunity to correct the non-compliance if the non-compliance is:
- Egregious, as determined by HHSC.
- Due to a substantiated allegation of fraud, waste, or abuse by the Office of Inspector General.
If a PSO does not respond to HHSC within the time frame specified in a notice of non-compliance, HHSC may:
- Require the EVV Aggregator reject all EVV visit transactions submitted from the EVV proprietary system until the PSO responds or corrects the non-compliance.
- Cancel the use of the EVV proprietary system without giving the PSO the opportunity to correct the non-compliance.
If HHSC cancels the use of a proprietary system, the PSO will be removed from the List of EVV Proprietary Systems Approved by HHSC.
Fraud, Waste and Abuse
Non-compliance with EVV standards and policy requirements may result in:
- Fraud, waste and abuse investigations.
- The recoupment of funds for any EVV claim paid or any overpayment based on inaccurate data.
HHSC may require the EVV Aggregator reject all EVV visit transactions submitted from an EVV proprietary system effective immediately if HHSC confirms an allegation of fraud, waste or abuse related to the functionality of the EVV proprietary system.
6000, EVV Visit Transaction
Revision 22-4; Effective Sept. 1, 2022
An EVV visit transaction is a record generated by an EVV system that contains data elements for an EVV visit.
The EVV visit transaction includes:
- Service authorization data
- Member data
- Service provider data
- Program provider or FMSA data
- EVV service delivery data
Once steps 1-3 as described in 4000 EVV System and Setup are complete, program providers, FMSAs or CDS employers are ready to begin using the EVV system.
The following steps explain how to use the EVV system and how the EVV system processes EVV visit transactions.
Step 4: Service providers and CDS employees must:
- Clock in at the beginning of service delivery using an approved clock in and clock out method.
- Clock out at the end of service delivery using an approved clock in and clock out method.
Step 5: The EVV system:
- Captures and verifies visit data. (Refer to 4400 Data Collection)
- Validates the identification and visit data against Texas Medicaid data.
- Notifies program providers, FMSAs or CDS employers of exceptions in the EVV visit transaction.
- Submits the EVV visit transaction to the EVV Aggregator.
Step 6: The EVV Aggregator:
- Conducts data validation.
- Determines if the EVV visit transaction is an accepted or rejected EVV visit transaction.
- Stores accepted EVV visit transactions for the claims matching process.
- Stores rejected EVV visit transactions and returns results to the EVV system.
Step 7: Program Providers, FMSAs and CDS employers complete visit maintenance, if necessary, to:
- Correct exceptions and rejected visit transactions sent back by the EVV aggregator.
- Adjust bill hours.
- Add reason codes and free text as required.
EVV Steps 4 through 7
Step 8: Program Providers and FMSAs use the EVV Portal to:
- Search and review visit data.
- Verify accepted EVV visits for billing.
- Access the claims matching results.
Step 9: Program Providers and FMSAs:
- Submit EVV claims to the appropriate claims management system.
Step 10: EVV Aggregator:
- Matches EVV claim line items to accepted EVV visit transactions.
- Returns EVV claims match result codes to the claims management system.
EVV Steps 8 through 10

6100 EVV System
Revision 22-4; Effective Sept. 1, 2022
The EVV system identifies exceptions and notifies program providers, FMSAs or CDS employers of any exceptions they must correct.
Each night the EVV system will send verified EVV visit transactions to the EVV Aggregator. Once the EVV Aggregator receives an EVV visit transaction, it will validate the data.
If the EVV visit transaction is rejected, the EVV system will receive a rejection code. The rejection code will be available in the EVV system and accessible by program providers, FMSAs or CDS employers, if applicable. Contact your EVV vendor or PSO for details on how to view rejection codes.
Program providers and FMSAs can use EVV Portal reports and search tools to identify EVV visit transactions they need to correct. Once corrected, the EVV system will re-send the EVV visit transaction to the EVV Aggregator for data validation.
Payers will not pay an EVV claim for reimbursement unless there is an accepted EVV visit transaction in the EVV Aggregator that matches the claim line item. Refer to 12200 Claims Matching.
6200 EVV Aggregator
Revision 21-1; Effective Nov. 1, 2021
The EVV Aggregator is a centralized database that collects, validates and stores statewide EVV visit transaction data transmitted by an EVV system.
Once the EVV Aggregator receives an EVV visit transaction from an EVV system, the EVV Aggregator:
- Conducts validation on data from the EVV visit transaction received from the EVV system.
- Stores all accepted and rejected EVV visit transactions.
- Accepts or rejects EVV visit transaction and returns results to the EVV system.
- Matches EVV claim line items to accepted EVV visit transactions in the EVV Aggregator and
- Sends claims match results to the claims management system for final processing by the appropriate payer.
6300 EVV Portal
Revision 21-1; Effective Nov. 1, 2021
The EVV Portal is an online system that allows users to perform searches and view reports associated with the EVV visit transaction data in the EVV Aggregator.
Program providers, FMSAs, MCOs and HHSC can search, view, print and export:
- EVV Portal Reports
- Accepted Visits
- Visit History
- EVV Claim Search
Note: CDS employers will not use the EVV Portal but will have access to EVV visit logs and related reports in the EVV system.
Program providers and FMSAs can:
- View accepted EVV visit transactions ready for billing.
- Access standard EVV reports and run queries on EVV visit data.
- Check the status and identify reasons for rejection of submitted EVV visit transactions.
7000, Clock In and Clock Out Methods
Revision 22-4; Effective Sept. 1, 2022
A service provider or CDS employee must use an HHSC-approved clock in and clock out method to begin and end service delivery when providing EVV services to a member in the home or the community.
EVV vendors offer the following three HHSC-approved clock in and clock out methods:
- Mobile method
- Home phone landline
- Alternative device
A PSO must offer one or more of the three HHSC-approved clock in and clock out methods listed above.
The PSO or EVV Vendor must provide access to clock in and clock out methods at no cost to the member, program provider, FMSA, CDS employer, service provider, HHSC, MCO or TMHP.
If the clock in and clock out method malfunctions, the EVV system must allow the program provider, FMSA or CDS employer to manually enter EVV visits.
When the service provider or CDS employee clocks in and clocks out using an HHSC-approved method, the EVV system captures the following visit data:
- The type of service provided (Service Authorization Data)
- The name of the recipient to whom the service is provided (Member Data)
- The date and times the provider began and ended the service delivery visit
- The location, including the address, where the service is provided
- The name of the person who provided the service (Service Provider Data)
7010 Manually Entered EVV Visits
Revision 22-4; Effective Sept. 1, 2022
A program provider, FMSA or CDS employer must manually enter an EVV visit into the EVV system when a service provider or CDS employee fails to clock in or out of the EVV system or an HHSC-approved clock in or clock out method is not available.
Manually entered visits will negatively impact the EVV Usage Score. Refer to 11000 Usage for more information.
The program provider, FMSA or CDS employer must complete the following steps if the service provider or CDS employee fails to clock in or out of the EVV system for any reason:
- Verify the service provider or CDS employee delivered services according to program policy and requirements.
- Receive and retain service delivery documentation from the service provider or CDS employee. Service delivery documentation should include:
- Program provider, FMSA and CDS employer name
- Member first and last name
- Member Medicaid ID
- EVV services delivered
- Date of the visit
- Actual Time In and Actual Time Out
- Service provider or CDS employee first and last name
- Location of the visit in the home or in the community
- Manually entering visits into the EVV system.
- Complete visit maintenance using the most appropriate Reason Code Number(s), Reason Code Description(s) and free text, if applicable.
- Ensure the visit transaction is accepted at the EVV Portal (applicable to program providers and FMSAs).
Program providers, FMSAs and CDS employers must complete all required visit maintenance including manually entering visits, within the visit maintenance time frame.
7020 Mobile Method
Revision 22-4; Effective Sept. 1, 2022
A service provider or CDS employee may use the mobile method for clocking in and out of the EVV system in the home or in the community. Each EVV vendor and PSO, if applicable, will supply a downloadable application for use on a smart phone or device with Internet connectivity.
If a service provider or CDS employee clocks in or out within 250 feet (EVV allowed geo-perimeter) of the member’s home, the default service delivery location is the member home. The service provider or CDS employee can select a different service delivery location if necessary.
If the service provider or CDS employee clocks in or out beyond the 250-foot EVV allowed geo-perimeter, the service provider or CDS employee must select a service delivery location.
Service Delivery Location options include:
- Member Home
- Family Home
- Neighbors Home
- Community
- Other
Note: If the service provider or CDS employee clocks in at the home, delivers services in the community and then clocks out at the home, the service delivery location would be member home.
Service providers may use their own personal smart phone or tablet, or a smart phone or tablet issued by the program provider.
Service providers must not use a member’s personal smart phone or tablet to clock in and clock out of the EVV system.
CDS employees may use:
- Their own personal smart phone or tablet
- A smart phone or tablet issued by the FMSA
- A smart phone or tablet owned by the CDS employer, if permission is granted.
The mobile method is the only clock in and clock out method the service provider or CDS employee may use when delivering EVV services in the community or when traveling out of state. Contact your program representative to determine if your service provider or CDS employee may deliver EVV services while the member is out of state.
The mobile method:
- Utilizes a secure login function for each user.
- Records the specific location at the exact time of clocking in and clocking out.
- Does not track location before clocking in, during service delivery or after clocking out.
- Does not use mobile device plan minutes and only uses minimal data.
- Does not store Protected Health Information (PHI) on the mobile device.
- Can be used when an internet connection or a cellular network is not available.
Note: EVV vendors cannot share or sell location data.
Clock in and clock out requirements:
- The program provider or FMSA must set up the mobile method in the member’s profile.
- The mobile device must be operational to use the mobile method. For example, the phone must be working, and the battery charged.
Service providers and CDS employees:
- Must follow instructions from their program provider, FMSA or CDS employer to download and activate the mobile application.
- Must obtain their own unique login credentials from their program provider, FMSA or CDS employer.
- Must only access the mobile application using their own login credentials.
- Must not share mobile application login credentials.
- May share the same mobile device for clocking in and clocking out of the EVV system for the same member using their own mobile application login credentials.
The program provider, FMSA or CDS employer may contact their EVV vendor or PSO, if applicable, for a full list of mobile application specifications, including supported mobile devices.
HHSC, TMHP, EVV vendors and MCOs are not liable for:
- Any cost incurred while using the mobile method.
- Any viruses on the mobile device.
- A hacked, broken, damaged, lost or stolen mobile device.
- A non-working mobile device.
7030 Home Phone Landline
Revision 22-1; Effective Jan. 7, 2022
The service provider or CDS employee may use the member’s landline, if the member agrees, for clocking in and clocking out of the EVV system. They do this by calling the EVV vendor’s or EVV PSO toll-free number.
If a member does not agree to allow the service provider or CDS employee to use their landline or if the member’s landline is frequently not available for the service provider or CDS employee to use, the service provider or CDS employee must use another approved clock in and clock out method.
Landline Requirements
- Program providers and FMSAs must follow the instructions from the vendor or EVV PSO to set up the landline.
- The landline must be the member’s home phone landline number or a landline in another location that the member frequently receives services, such as a family member’s home or a neighbor’s home.
- The owner of the landline must give permission to the member and the service provider or CDS employee to use the telephone for EVV.
- The phone must be a landline phone. It must not be an unallowable landline phone type. See Unallowable Landline Phone Type below.
Program Providers and FMSAs are responsible for initial setup and maintenance of the landline in the EVV system. The program provider or FMSA must:
- Enter the member’s landline number in the EVV system before the service provider or CDS employee can use the landline to clock in and clock out.
- Enter one or more landline number if the member frequently receives services in an alternate location.
- Verify the landline number using the EVV Landline Phone Verification Report located in the EVV system.
- Ensure the landline number(s) listed in the member’s profile are current.
The program provider or FMSA must update the member’s profile in the EVV system if the landline number used for clocking in and clocking out does not match.
Unallowable Landline Phone Type
An unallowable landline phone type is a mobile phone number or cellular enabled phone number. Phones used to clock in or clock out through the landline method must be a landline phone, and not a cellular phone or device.
Unallowable landline phone types include:
- Cellular phones
- Cellular enabled devices such as tablets and smart watches
Numbers from phone carriers such as Cricket, that provide mobile phone services only will always be identified as an unallowable phone type.
Note: If the service provider or CDS employee wants to use a cell phone or tablet, they must use the mobile method.
Identification of an Unallowable Landline Phone Type
Program providers, FMSAs and CDS employers must use the EVV Landline Phone Verification Report in the EVV system to identify an unallowable landline phone type as “mobile”. Payers will also use this report to conduct EVV Landline Phone Verification Reviews, refer to 10020 EVV Landline Phone Verification Reviews.
If the program provider, FMSA, CDS employer or payer identify an unallowable phone type, action must be taken.
Program Provider Required Actions
When an unallowable phone type is identified, program providers must either:
- Verify and document that the phone type is an allowable phone type; or
- Remove the unallowable landline phone type from the EVV system as the member’s home phone landline and ensure a valid landline or another approved clock in and clock out method is used.
Program providers must follow any actions required by the payer in a notice of non-compliance.
FMSA and CDS Employer Required Actions
When an unallowable phone type is identified, FMSAs must notify the CDS employer that the phone number is an unallowable landline phone type and:
- Work with the CDS employer to verify and document that the phone type is an allowable phone type; or
- Remove the unallowable landline phone type from the EVV system as the member’s home phone landline and work with the CDS employer to ensure a valid landline number or another approved clock in and clock out method is used.
When an unallowable phone type is identified, CDS employers must take one of the following actions:
- provide documentation to the FMSA demonstrating the current landline number is an allowable phone type;
- provide a valid landline number to the FMSA; or
- choose another approved clock in and clock out method for the CDS employee to use and inform the FMSA of the new method.
FMSAs and CDS employers must follow any actions required by the payer in a notice of non-compliance.
Documentation
When requested by the payer, program providers and FMSAs must provide documentation to:
- demonstrate that the phone number is from an allowable phone type; or
- demonstrate that that the service provider or CDS employee is no longer using an unallowable landline phone type.
Examples of documentation from an external source showing that the phone number is an allowable landline phone type, may include but not limited to screenshots or printouts from:
- White Pages
- Free Carrier Look-up Service
- Reverse Phone Check
If the phone number is from an unallowable phone type, program providers and FMSAs must provide documentation showing the service provider or CDS employee is no longer using an unallowable landline phone type. Acceptable documentation includes one of the following:
- A screenshot of the member profile reflecting another approved clock in and clock out method is used.
- Verification from the EVV system showing that an alternative device was ordered for the member, if applicable.
7040 Alternative Device
Revision 22-4; Effective Sept. 1, 2022
An alternative device is an HHSC-approved electronic device that allows a service provider or CDS employee to clock in and out of the EVV system from the member’s home.
A program provider, CDS employer or service provider must explain to the member the purpose of the alternative device and how the alternative device works.
The alternative device produces codes that identify the precise date and time service delivery begins and ends. Codes from alternative devices, provided by EVV vendors, expire seven days from the date of the EVV visit. Codes from alternative devices must be entered in to the EVV system before they expire by calling a toll-free number provided by the EVV vendor.
The service provider or CDS employee may use any phone type to call the toll-free number and enter the alternative device codes. However, service providers or CDS employees should never use or request to use the member’s mobile phone unless the member is a CDS employer and the CDS employer has given the CDS employee permission to use the CDS employer’s mobile phone.
The program provider or FMSA must document in the member’s case file each time the alternative device is damaged or lost. The program provider, FMSA or CDS employer must also order a new alternative device or ensure another clock in and clock out method is used.
If the alternative device was damaged or lost by a member then the program provider, FMSA or CDS employer is responsible for requesting:
- An interdisciplinary team (IDT) meeting.
- A service planning team (SPT) meeting.
- A child and family team (CFT) meeting or a meeting with the member, their LAR and any natural or formal support to discuss the use of the alternative device with the member.
Failure to document a lost or damaged alternative device in the member’s case file or schedule an IDT, SPT or CFT meeting with the member may result in the payer or the EVV vendor holding the program provider or FMSA responsible for the lost or damaged alternative device.
The alternative device must always remain in the member’s home even during an evacuation. If the alternative device does not remain in the home, the payer may make a Medicaid fraud referral to the HHS Office of the Inspector General.
Note: A PSO may offer different types of alternative devices. All alternative devices must support the collection of critical data elements. HHSC must approve any alternative device used by the PSO before use. Refer to 5060 EVV Proprietary System General Operations and 4400 Data Collection.
Ordering an Alternative Device from an EVV vendor
Once the program provider, FMSA or CDS employer has determined a member needs an alternative device, they have 10 business days to order an alternative device from the EVV vendor.
Program providers, FMSAs on behalf of a CDS employer, or CDS employers can order an alternative device through an EVV vendor. The EVV vendor will provide instructions on how to order a device.
The EVV vendor has 10 business days to process and ship the alternative device to the requestor upon receipt of a complete order. Depending on the shipping method, it may take additional days to deliver the order.
If a clock in or clock out method is not available for the service provider or CDS employee to use prior to the delivery of an alternative device, the service provider or CDS employee must manually document the EVV visit and submit service delivery documentation to the program provider or FMSA. The program provider or FMSA must manually enter visit data in the EVV system within the visit maintenance time frame.
Using the EVV vendor electronic ordering method, program providers, FMSAs on behalf of CDS employers, or CDS employers can:
- Order a new or replacement alternative device
- Track orders for the alternative device
- Manage, assign and un-assign alternative devices
- Manage shipping addresses
If a member does not want an alternative device in their home and another HHSC- approved clock in and clock out method is not available:
- The program provider or FMSA must document the reason in the member’s case file.
- An IDT, SPT or CFT meeting must be conducted.
Installing an Alternative Device
The program provider, CDS employer, service provider or CDS employee must:
- Ask the member where to place the alternative device in the member’s home. The alternative device:
- Should be in a location where it is always accessible to the service provider or CDS employee.
- May be attached using a zip tie.
- Must not be mounted in a location that may be dangerous to a member or cause damage to the member’s home.
- Install the alternative device by placing the device in the member’s home for use by the service provider or CDS employee.
Examples of places where the alternative device may be located in the member’s home:
- Kitchen counter
- Coffee table
- Lockbox located in the garage or on the patio
Malfunctioning Alternative Device
The service provider or CDS employee must notify the program provider or CDS employer immediately if the alternative device malfunctions or fails to generate codes.
When the service provider or CDS employee notifies the program provider or CDS employer the alternative device has malfunctioned:
- The service provider or CDS employee must manually document the EVV visit and submit service delivery documentation to the program provider, FMSA or CDS employer for manual entry of an EVV visit. Refer to 1400 Failure to use an EVV System.
- The program provider, FMSA or CDS employer must contact the EVV vendor or PSO to report the malfunctioning device and order a replacement alternative device.
Equipment provided by an HHSC-approved EVV vendor, must be returned when the equipment is no longer used.
7050 Using Multiple Clock In and Clock Out Methods
Revision 22-4; Effective Sept. 1, 2022
A service provider or CDS employee may use multiple clock in and clock out methods.
Examples of using one method to clock in and out for a single EVV visit happens when the service provider or CDS employee:
- Clocks in and out using the mobile method.
- Clocks in and out using a home phone landline.
- Clocks in and out using an alternative device.
Examples of using multiple methods to clock in and out for a single EVV visit happens when the service provider or CDS employee:
- Clocks in using a home phone landline and clocks out using the mobile method.
- Clocks in using the mobile method and clocks out using a home phone landline.
Program providers and CDS employers may contact their EVV vendor or PSO for more information about which methods can be used together or for EVV system training.
7060 EVV Services Delivered Outside the Member’s Home
Revision 22-4; Effective Sept. 1, 2022
The mobile method is the only HHSC-approved clock in and clock out method when an EVV service begins or ends in the community. Using the mobile method for clocking in and out in the community avoids negative impacts to the EVV Usage Score. Refer to 10010 EVV Usage Reviews for more information.
If a service provider or CDS employee is unable to use the mobile method when an EVV service begins or ends in the community, they must document visit data per program policy and 1400 Failure to Use an EVV System.
Program providers and CDS employers may contact their EVV vendor or PSO for more information and EVV system training.
8000, Visit Maintenance
Revision 22-4; Effective Sept. 1, 2022
Visit maintenance is the process used by the program provider, FMSA or CDS employer to correct an EVV visit transaction in the EVV system to accurately reflect the delivery of service.
Program providers, FMSAs or CDS employers must complete all required visit maintenance. They must also ensure the EVV Aggregator accepts the visit transaction before the program provider or FMSA submits an EVV claim. If more visit maintenance is completed after submitting an EVV claim, program providers or FMSAs must submit an adjusted claim to match the updated visit transaction.
If the program provider or FMSA submits an EVV claim before required visit maintenance is complete, a payer may deny or recoup the EVV claim as part of contract oversight.
If the program provider or FMSA delegates visit maintenance responsibilities to a:
- Third party such as a subcontractor, the program provider or FMSA is always responsible for actions taken by the third party.
- Third party, the program provider or FMSA ensures the third party follows all privacy and security protocols, including when the subcontractor or third-party accesses EVV data.
If CDS employers delegate visit maintenance responsibilities to their designated representative (DR), the CDS employer is responsible for any actions taken by their DR. They must ensure that the DR follows all privacy and security protocols, including when the DR accesses EVV data.
8010 Required Visit Maintenance
Revision 22-4; Effective Sept. 1, 2022
Program providers, FMSAs or CDS employers must complete visit maintenance when the:
- EVV system cannot “auto-verify” a visit transaction.
- EVV system identifies exceptions and critical errors.
- EVV Aggregator rejects the EVV visit transaction due to incorrect or missing data.
- Program provider, FMSA or CDS employer reduces bill hours after the EVV system auto-verifies the EVV visit transaction.
- EVV system is unavailable.
- Service provider or CDS employee fails to use the EVV system.
Exceptions are identified by an EVV system and prevent an EVV visit transaction from being auto-verified or sent to the EVV Aggregator.
Refer to 1400 Failure to Use an EVV System and 6000 EVV Visit Transaction for more information.
8020 Auto-Verification
Revision 22-4; Effective Sept. 1, 2022
Auto-Verification
Each time a service provider or CDS employee clocks in or clocks out during service delivery, the EVV system will:
- Capture visit data.
- Verify the clock in and clock out method.
- Compare critical data elements, including schedule data if applicable, in the EVV system.
If all visit data and identification data in the EVV system match, the system auto-verifies the EVV visit transaction which means there were no exceptions found.
Refer to 4610 Schedule Types for information about how auto-verification works for each schedule type.
If an EVV visit transaction is missing a clock in or a clock out and requires manually entered visit data, or if the data captured at the time of clock in or out does not match the critical data elements in the EVV system, the system cannot auto-verify an EVV visit transaction and will notify the program provider, FMSA or CDS employer of an exception.
Clearing Exceptions
The EVV system may generate one or more exceptions when the system cannot auto-verify the visit data captured at the time of clock in or clock out.
To clear an exception, program providers, FMSAs or CDS employers must complete visit maintenance in the EVV system by:
- Updating the identification or visit data for a member, if applicable. Refer to 4400 Data Collection for more information.
- Selecting the most appropriate EVV reason code(s), if required.
- Confirming the EVV visit.
Selecting the most appropriate EVV reason code(s) explains the reason for completing visit maintenance. The process involves:
- Selecting an EVV Reason Code Number.
- Selecting an EVV Reason Code Description.
- Entering required free text, if applicable.
Refer to 9000 EVV Reason Codes and Current HHSC EVV Reason Codes for more information.
The following are some examples that describe when the EVV system will not auto-verify an EVV visit:
- Clock in or out time is missing
- Clock in or out time does not match a schedule entered in the EVV system
- An EVV visit is manually entered in to the EVV system
- Service providers or CDS employees clock in or clock out using a landline phone not registered in the member’s profile
Auto-Verification without a Schedule
If no schedule is entered in the EVV system, the EVV system will validate the following critical data elements:
- Identity of the service provider or CDS employee
- Identity of the member
- Actual hours worked
- Clock in and out method(s)
- Service type for the visit
If the above data elements match the data in the member’s profile, the visit will auto-verify without exceptions.
If any of the above data elements do not match, the EVV system will not auto-verify the EVV visit and visit maintenance must be completed.
8030 EVV System Validation
Revision 22-1; Effective Jan. 7, 2022
Once the EVV system has verified a visit, it will conduct more system validation checks on the EVV visit transaction before sending the EVV visit transaction to the EVV Aggregator.
The EVV system validation ensures the identification data and visit data is in the correct format. It compares the critical data elements to Texas Medicaid data stored at TMHP.
An EVV system must perform the following validation before sending an EVV visit transaction to the EVV Aggregator:
- Verifies that no required visit data elements are missing.
- Verifies that all required visit data elements are in the correct format (length, alphanumeric, only valid values).
- Verifies that all required identification data elements are in the correct format (NPI, API, Provider Number).
- Verifies the service group and service code or HCPCS and modifier combination is valid for the member or EVV visit transaction.
If an EVV visit transaction fails the system validation, the EVV system will:
- Not send the EVV visit transaction to the EVV Aggregator.
- Notify the program provider, FMSA or CDS employer of the exceptions that must be corrected.
To clear EVV system validation exceptions, the program provider, FMSA or CDS employer must complete visit maintenance. Once the program provider, FMSA or CDS employer clears the exceptions, the EVV system will send the EVV visit transaction to the EVV Aggregator for final processing.
8040 EVV Aggregator Validation
Revision 22-1; Effective Jan. 7, 2022
The EVV Aggregator performs many validations of all data elements on the EVV visit transaction. The EVV Aggregator validations include verifying the:
- NPI or API for the program provider or FMSA to ensure it is active for the visit date.
- Provider number is valid for the NPI or API on the visit date.
- Member’s payer matches the Medicaid data.
- Member has Medicaid eligibility for the visit date.
- Service group, service code or HCPCS and Modifier on the visit date.
Based on the above validations, the EVV Aggregator will either accept or reject the EVV visit transaction received from an EVV system then display the status in the EVV Portal.
After the EVV Aggregator accepts an EVV visit transaction, the program provider or FMSA can submit an EVV claim associated with the EVV visit transaction.
When the EVV Aggregator rejects an EVV visit transaction, the EVV Aggregator returns the EVV visit transaction to the EVV system with the reason for the rejection. The program provider, FMSA or CDS employer must complete visit maintenance. After visit maintenance is complete the program provider or FMSA must resubmit the EVV visit transaction to the EVV Aggregator.
8050 Visit Maintenance Time Frame
Revision 22-4; Effective Sept. 1, 2022
Program providers, FMSAs and CDS employers must complete all required visit maintenance, including entry of manual EVV visits, within 95 days from the date of service delivery. This is known as the visit maintenance time frame. HHSC may extend the visit maintenance time frame as needed.
After the visit maintenance time frame has expired, the EVV system locks the EVV visit transaction and program providers, FMSAs or CDS employers may only complete visit maintenance if the payer approves a Visit Maintenance Unlock Request.
8060 Visit Maintenance Unlock Request
Revision 22-4; Effective Sept. 1, 2022
A Visit Maintenance Unlock Request, when approved, allows a program provider, FMSA or CDS employer the opportunity to correct data element(s) on an EVV visit transaction(s) after the visit maintenance time frame has expired.
The program provider, FMSA or CDS employer may request a payer unlock EVV visit transaction(s) for visit maintenance. If a request is submitted by an FMSA, the FMSA must ensure the CDS employer approves any corrections to time worked. If the request is submitted by a CDS employer, the CDS employer must notify their FMSA in writing (e.g., email).
Approvals and denials of Visit Maintenance Unlock Requests are at the payer’s discretion and are determined on a case-by-case basis based on EVV policy or EVV system error. If the request is submitted by the CDS employer and the payer has approved or denied the request, the payer must also notify the FMSA in writing (e.g., email).
Payers will only approve requests to manually enter and export an EVV visit after the visit maintenance time frame if:
- The program provider was unable to manually enter and export an EVV visit during the visit maintenance time frame because of a payer or EVV vendor system error, and the error was not resolved within the visit maintenance time frame.
- The CDS employer, or the FMSA on behalf of the CDS employer, was unable to manually enter and export an EVV visit during the visit maintenance time frame because of a payer, EVV vendor system, or EVV proprietary system error, and the error was not resolved within the visit maintenance time frame.
- HHSC determines an exception is required for circumstances such as a natural disaster.
When submitting a Visit Maintenance Unlock Request to create a manual visit due to a payer or EVV system error, the program provider, FMSA or CDS employer must provide evidence demonstrating:
- They informed the payer of the error within the visit maintenance time frame.
- The error was not resolved during the visit maintenance time frame.
- They made a good faith effort to comply with the visit maintenance time frame.
Making corrections to EVV visit transactions during a LTC FFS contract monitoring review or after it has occurred will not change any type of contract action such as recoupment or settlement reviews taken as result of the LTC FFS contract monitoring review.
Visit Maintenance Unlock Request Process
Program providers, FMSAs and CDS employers must complete the Visit Maintenance Unlock Request specific to their payer and service delivery option found on their payer’s website.
Emails sent with a completed Visit Maintenance Unlock Request must be sent securely and include a contact name, email address and phone number.
The program provider or FMSA can only select the following items from the ‘Incorrect Data Element’ column of their Visit Maintenance Unlock Request to be unlocked for correction:
- Bill Hours
- Contract Number
- Employee ID
- HCPCS Code/Modifier
- Member Medicaid ID
- NPI/API
- Payer
- Reason Code
- Service Code
- Service Group
- Units
- Visit Location
- N/A – Export Only
The CDS employer can only select the following items from the ‘Incorrect Data Element’ column of their Visit Maintenance Unlock Request to be unlocked for correction:
- Bill Hours
- Employee ID
- HCPCS Code/ Modifier
- Member Medicaid ID
- Payer
- Reason Code
- Service Code
- Service Group
- Units
- Visit Location
- N/A – Export Only
Initial Request to Payer
Payers must process Visit Maintenance Unlock Requests after receiving a secure and complete request from the program provider, FMSA or CDS employer within the following time frames:
- Ten business days
- Thirty business days if the request was submitted as supporting documentation for a MCO claims appeal
Email requests not sent securely will result in the payer denying the request due to a violation of the Health Insurance Portability and Accountability Act.
Contact the payer for assistance with sending a secure email request.
Payer Request for More Information
The payer may request more information from the program provider, FMSA or CDS employer, the request must be fulfilled within the following time frames of receipt:
- Ten business days
- Fifteen business days if the request is part of a MCO claims appeal.
If the program provider, FMSA or CDS employer does not fulfill the request within the established time frames, the payer may deny the request and a new Visit Maintenance Unlock Request must be submitted.
Payer Denial of Request
If the payer denies the request, the payer must notify the program provider, FMSA or CDS employer through email with the reason for the denial. The email notification must include at a minimum the following information on how to:
- Submit a new Visit Maintenance Unlock Request
- Request a claims appeal, if applicable
- Submit a formal complaint against the payer
Payers may automatically deny a Visit Maintenance Unlock Request if the request:
- Was not sent through a secure method
- Is incomplete or missing required information
- Could not be unencrypted
- Was submitted using an outdated or modified version of the Visit Maintenance Unlock Request
Payer Approval of Request
If the payer approves the Visit Maintenance Unlock Request, the payer will send the approved Visit Maintenance Unlock Request to the EVV vendor or PSO.
Only approved items on the Incorrect Data Element column of the Visit Maintenance Unlock Request will be unlocked for editing.
EVV vendors or PSOs must only allow changes to the items approved by the payer.
Payer Incorrect, Incomplete or Retroactive Authorization Approvals
The payer must approve the Visit Maintenance Unlock Request when:
- The payer previously provided incorrect or incomplete information on the prior authorization for a member and the updated authorization requires updates to EVV visit transactions outside of the EVV visit maintenance time frame.
- The payer submits a retroactive authorization for a member that will require the program provider, FMSA or CDS employer to resubmit an EVV visit transaction or EVV claim outside of the EVV visit maintenance time frame.
- HHSC directs the payer to approve within the initial request time frame specified in this policy.
EVV Vendor and EVV PSO Approval and Denial
Once the EVV vendor or PSO receives the approved Visit Maintenance Unlock Request from the payer, the EVV vendor or EVV PSO must validate the information submitted.
Once the information is validated:
- The EVV vendor has 10 business days from receipt of the approved Visit Maintenance Unlock Request to complete visit maintenance or schedule a meeting with the program provider, FMSA or CDS employer to complete visit maintenance.
- The PSO must complete visit maintenance within 20 business days from receipt of the approved Visit Maintenance Unlock Request.
If the information submitted by the program provider, FMSA or CDS employer is incorrect, invalid or missing data elements, the EVV vendor or PSO will:
- Not unlock EVV visit transaction(s) for visit maintenance.
- Return the Visit Maintenance Unlock Request to the program provider, FMSA or CDS employer.
- Notify the payer, program provider, FMSA or CDS employer of the reason the EVV visit transaction(s) cannot be unlocked for visit maintenance.
EVV vendors and payers cannot provide specific information about what data elements should be updated. The EVV vendor can direct the program provider, FMSA or CDS employer to the visit dates and members that are approved within the Visit Maintenance Unlock Request and provide education about the EVV system.
Once the information is corrected, the program provider, FMSA or CDS employer must submit a new Visit Maintenance Unlock Request to the payer.
Refer to the EVV webpage for the Visit Maintenance Unlock Request Job Aid for program providers, FMSAs or CDS employers.
8070 Visit Maintenance and Billing EVV Claims
Revision 22-4; Effective Sept. 1, 2022
A program provider, FMSA and CDS employer must ensure all required data elements are correct and visit maintenance is complete before the program provider or FMSA submit an EVV claim to the appropriate claims management system.
If the program provider, FMSA or CDS employer needs to complete visit maintenance on an accepted EVV visit transaction that has already been billed, the program provider or FMSA must:
- Complete visit maintenance on the EVV visit transaction(s).
- Ensure the EVV Aggregator accepts the corrected EVV visit transaction.
- Resubmit the EVV claim per the payer’s corrected claim process (e.g. negative bill the original claim and resubmit a corrected claim).
The EVV Visit Maintenance Unlock Request does not override the timely filing deadline for submission of a new or corrected claim. If an exception to the timely filing deadline is needed, program providers or FMSAs must follow the process of their payer.
8080 Last Visit Maintenance Date
Revision 22-1; Effective Jan. 7, 2022
The Last Visit Maintenance Date field on the EVV visit transaction identifies the last date visit maintenance was completed. Payers may review the Last Visit Maintenance Date on the EVV visit transaction and the date and time TMHP received the associated EVV claim.
If the Last Visit Maintenance Date is after the EVV claim receipt date, the EVV claim is subject to recoupment. To avoid recoupment, program providers and FMSAs must submit an adjusted claim if visit maintenance is completed after initial claim submission.
The EVV system will update the Last Visit Maintenance Date when any of the following fields are updated:
- API/NPI
- Contract number
- Member Medicaid ID
- Service group
- Service code
- HCPCS code
- Modifier
- Bill hours
- Units
- Adding a Reason Code number
- Adding a Reason Code description
- Entering Reason Code free text
The program provider or FMSA may review the Last Visit Maintenance Date on the EVV Visit Log Report and the EVV visit detail screen located in the EVV Portal.
8090 Rounding Rules
Revision 22-1; Effective Jan. 7, 2022
The EVV system calculates bill hours on an EVV visit transaction by rounding the actual hours worked to the nearest quarter hour increment.
The EVV system rounds up to the next quarter hour increment when the actual hours worked are eight minutes or more than the previous quarter hour increment. The EVV system rounds down to the previous quarter hour increment when the actual hours worked are seven minutes or less from the previous quarter hour.
| Actual Hours Worked | Quarter Hour Increment | Bill Hours |
|---|---|---|
| 0 - 7 minutes | 0 minutes | 0.00 |
| 8 - 22 minutes | 15 minutes | 0.25 |
| 23 - 37 minutes | 30 minutes | 0.50 |
| 38 - 52 minutes | 45 minutes | 0.75 |
| 53 - 67 minutes | 60 minutes or 1 hour | 1.00 |
Rounding rules examples:
- If a service provider works two hours and 53 minutes of actual hours for a shift, the bill hours will round up to three hours.
- If a service provider works two hours and 52 minutes of actual hours for a shift, the bill hours will round down to 2.75 hours.
- If a service provider works four hours and 10 minutes of actual hours for a shift, the bill hours will round up to 4.25 hours.
- If a service provider works four hours and six minutes of actual hours for a shift, the bill hours will round down to four hours.
The EVV system does not round each clock in or clock out time. The EVV system only rounds the total duration of the actual hours worked for each visit.
The program provider, FMSA or CDS employer may downward adjust bill hours if the actual hours worked, captured in the EVV system, are incorrect or if the program provider or FMSA intends to bill Medicaid for less time than actual hours worked in the EVV system.
The program provider, FMSA or CDS employer may never increase bill hours beyond the actual hours worked.
Program providers and FMSA must bill according to the EVV Service Bill Codes Table and follow program rules and policies, including any more program or MCO requirements regarding rounding.
8100 Visit Maintenance Reduction Features
Revision 22-3; Effective June 1, 2022
Visit maintenance reduction features help to reduce visit maintenance and increase auto-verification of an EVV visit transaction.
Program providers and FMSAs who enter Daily Fixed or Daily Variable schedule types in the EVV system can turn on and off visit maintenance reduction features based on the selected schedule type. If an EVV PSO implements schedule types in their HHSC-approved EVV system, the EVV PSO may also implement visit maintenance reduction features.
Visit maintenance reduction features only apply when a schedule is entered in the EVV system. Refer to 4600 Schedules for more information.
Contact your EVV vendor to learn more about visit maintenance reduction features in the EVV system.
Optional Expanded Time for Auto-Verification
The Optional Expanded Time for Auto-Verification is a feature that the program provider or FMSA can turn on in the EVV system. When this feature is turned on, the EVV system will auto-verify an EVV visit transaction if the duration of service delivery is no more than .25 bill hours greater or less than the scheduled duration with no exceptions or critical errors.
An example of a scheduled EVV visit auto-verifying:
- The schedule in the EVV system is 1 to 3 p.m., the duration of the scheduled visit is two hours.
- The program provider or FMSA has turned on the Optional Expanded Time for Auto-Verification in the EVV system.
- The service provider or CDS employee clocked in at 12:45 p.m. and clocked out at 3 p.m.
- The actual hours worked are two hours and 15 minutes which rounds to 2.25 bill hours.
- The EVV system will auto-verify because 2.25 bill hours is .25 bill hours greater than the scheduled duration.
An example of a scheduled EVV visit not auto-verifying:
- The schedule in the EVV system is 1 to 3 p.m., the duration of the scheduled visit is two hours.
- The program provider or FMSA has turned on the Optional Expanded Time for Auto-Verification in the EVV system.
- The service provider or CDS employee clocked in at 12:45 p.m. and clocked out at 3:09 p.m.
- The actual hours worked are two hours and 24 minutes which rounds to 2.50 bill hours.
- The EVV system will not auto-verify because 2.50 bill hours is not within .25 bill hours of the scheduled duration.
Optional Automatic Downward Adjustment
The Optional Automatic Downward Adjustment is a feature that the program provider or FMSA can turn on to automatically downward adjust bill hours by .25 to match the duration of the scheduled visit. This feature is only available if the program provider or FMSA also turns on the Optional Expanded Time for Auto-Verification feature in the EVV system.
The Optional Automatic Downward Adjustment feature only applies to bill hours and does not change actual hours worked.
For example:
- The schedule in the EVV system is 1 – 3 p.m., the duration of the scheduled visit is two hours.
- The program provider or FMSA has turned on the Optional Automatic Downward Adjustment and Optional Expanded Time for Auto-Verification.
- The service provider or CDS employee clocked in at 12:45 p.m. and clocked out at 3 p.m.
- The actual hours worked are two hours and 15 minutes which rounds to 2.25 bill hours.
- 2.25 bill hours is within .25 bill hours of the scheduled duration.
- The EVV system will auto-verify and automatically downward adjust the bill hours to 2.00.
Program providers, FMSAs or CDS employers must ensure the member’s plan of care is followed. Although visit maintenance reduction features are available and add flexibility, the needs of the member must always come first.
For example, if a member needs their service provider or CDS employee to be at the home at the scheduled time of 8 a.m. to receive help getting out of bed, the service provider or CDS employee must be there on time. The program provider, FMSA and CDS employer must document all situations as needed and in accordance with program policy and licensure requirements.
9000, EVV Reason Code
Revision 22-4; Effective Sept 1, 2022
Reason Code Number(s) represent the overall issue for the need to complete visit maintenance on an EVV visit transaction. Reason Code Description(s) provide more detail about why visit maintenance was completed.
Program providers, FMSAs or CDS employers must select the most appropriate Reason Code Number(s), Reason Code Description(s) and must enter any required free text when completing visit maintenance in the EVV system.
If an EVV visit transaction is missing a clock in or clock out, program providers, FMSAs or CDS employers must use Reason Code Number 900 Non-Preferred, the appropriate Reason Code Description(s), and any other applicable EVV reason code.
Program providers, FMSAs and CDS employers can use multiple Reason Code Numbers and Reason Code Descriptions to clarify more than one exception when completing visit maintenance on a single visit.
See current HHSC EVV Reason Codes located on the EVV webpage for Reason Code Number(s), Reason Code Description(s) and required free text that must be documented for each reason code.
9010 EVV Reason Code Free Text Requirements
Revision 21-1; Effective Nov. 1, 2021
Free text is additional information the program provider, FMSA or CDS employer enters to further describe the need for visit maintenance.
Program providers, FMSAs or CDS employers completing visit maintenance in the EVV system must enter additional information in the free text field when:
- The visit is missing a clock in time, a clock out time or both.
- Enter the actual missing clock in or clock out time
- Using the following Reason Code Numbers:
- 131-Emergency
- 600-Other
- 900-Non-preferred
See the current HHSC EVV Reason Codes table for the free text requirement that must be documented for each reason code.
Compliance
Failure to document required free text may result in enforcement actions including recoupment of associated claim(s).
The Required Free Text Review may begin on or after the visit maintenance time frame has expired. This is to review the entry of required free text when a clock in or clock out is missing and when the following Reason Code Numbers are used:
- 131-Emergency
- 600-Other
- 900-Non-preferred
Refer to 10000 EVV Compliance Reviews for more information.
The table below lists examples of required free text.
| Reason for Visit Maintenance | Reason Code Number | Free Text Required (Examples) |
|---|---|---|
| Missing Clock In Time |
900 A: Failure to call in 200 A: Alternative device ordered |
|
| Missing Clock Out Time |
900 B: Failure to call out 300 A: Phone lines not working |
|
| Missing Clock In and Clock Out Time |
900 C: Failure to call in and out 130 C: Ice or Snow storm |
|
| Emergency | 131 |
|
| Other | 600 |
|
10000, EVV Compliance Reviews
Revision 22-4; Effective Sept. 1, 2022
Payers conduct EVV compliance reviews to ensure program providers, FMSAs and CDS employers are in compliance with EVV requirements and policies.
Payers will not start reviews until the visit maintenance time frame has expired.
Payers will conduct reviews and initiate contract or enforcement action if the program providers, FMSAs or CDS employers do not meet any of the following EVV compliance requirements:
- EVV Usage
- Meet the minimum EVV Usage Score
- EVV Landline Phone Verification
- Ensure valid phone type is used
- EVV Required Free Text (excluding the CDS option until further notice as determined by HHSC.)
- Document required free text
Refer to 7000 Clock In and Clock Out Methods, 9000 EVV Reason Code, and 11000 Usage for more information.
HHSC may change compliance requirements due to a natural disaster or at the discretion of HHSC.
Compliance Grace Periods
If program providers, FMSAs and CDS employers do not meet any of the EVV compliance requirements during the compliance grace period, payers will not initiate enforcement action unless noted by HHSC.
Payers will post a notice on their websites 90 days prior to the start of reviews.
During the Compliance Grace Periods
Program providers and FMSAs must monitor compliance reports monthly, at a minimum, in the EVV portal and perform the following:
- Use the EVV system as required
- Establish a process to monitor compliance reports with their CDS employer (if Option 3 on Form 1722, Employers Selection for Electronic Visit Verification Responsibilities) unless the CDS employer has read only access in the EVV system
- Complete all required visit maintenance before billing
- Train or re-train service providers on clock in and clock out methods (Specific to program providers only. Refer to 4240 Training Requirements for Service providers and CDS Employees)
- Ask questions
The CDS employer must monitor compliance reports monthly, at a minimum, in the EVV system and perform the following:
- Use the EVV system as required
- Complete all required visit maintenance (if Option 1 on Form 1722, Employers Selection for Electronic Visit Verification Responsibilities)
- Establish a process to monitor compliance reports with their FMSA (if Option 3 on Form 1722, Employers Selection for Electronic Visit Verification Responsibilities) unless they have read only access in the EVV system
- Train or re-train CDS employees on clock in and clock out methods
- Ask questions
State-Required Personal Care Services Grace Period
State-Required Personal Care Services are personal care services provided by program providers required to use EVV in 2016 or earlier per Texas Government Code, Section 531.024172.
The grace period dates of service for program providers started Sept. 1, 2019 and ended Aug. 31, 2020 and included:
- EVV Usage Reviews
Cures Act Personal Care Services Grace Period
Cures Act Personal Care Services are personal care services provided by program providers, FMSAs and CDS employers required to use EVV by Jan. 1, 2021 per the 21st Century Cures Act.
The grace period dates of service for program providers, FMSAs and CDS employers started Jan. 1, 2021 and ended Dec. 31, 2021 and includes:
- EVV Usage Reviews (Program provider and FMSA only)
- EVV Landline Phone Verification Reviews
- EVV Required Free Text Reviews (excluding the CDS option until further notice as determined by HHSC)
Due to availability of the EVV CDS Employer Usage report, the grace period dates of service for CDS employer EVV Usage Reviews started Jan. 1, 2021 and ended Aug. 31, 2022 unless noted by HHSC.
See Personal Care Services required to use EVV (PDF) on the EVV webpage for the complete list of services included in each grace period.
10010 EVV Usage Reviews
Revision 22-4; Effective Sept. 1, 2022
Payers review the EVV Usage Score quarterly.
EVV Usage Reviews are conducted after the visit maintenance time frame has expired based on the last date of the quarter to determine compliance.
The EVV Usage Score measures manually entered EVV visit transactions and rejected EVV visit transactions.
A manually entered EVV visit transaction is an EVV visit that is manually entered into the EVV system when a service provider or CDS employee fails to use the EVV system to clock in when service delivery begins, clock out when service delivery ends, or both.
A rejected EVV visit transaction is an EVV visit transaction that is exported from an EVV system to the EVV Aggregator but is not accepted by the EVV Aggregator.
Refer to 8000 Visit Maintenance and 11000 Usage for more information.
Program Providers
The payers will use the EVV Usage Report (located in the EVV Portal) to determine the EVV Usage Score for each program provider’s contract with HHSC and the MCOs.
FMSAs
The payers will use the EVV FMSA Usage Report (located in the EVV Portal) to determine the EVV Usage Score for each FMSAs contract with HHSC and the MCOs.
CDS Employers
The payers will use the EVV CDS Employer Usage Report (located in the EVV Portal and the EVV System) to determine the EVV Usage Score for each Medicaid member that selects the CDS option with HHSC or an MCO.
Refer to 11000 Usage for more information.
Failure to Meet the Compliance Standard
Failure to meet the compliance standard may result in the following actions.
Program Provider and FMSA Enforcement Actions
When a program provider or FMSA fails to meet and maintain the minimum EVV Usage Score of 80% in a state fiscal year quarter, the payer may send a notice of non-compliance to enforce one or more of the following progressive enforcement actions based on the number of occurrences within a 24-month period:
- First occurrence within a 24-month period - Require more EVV policy, system and portal trainings within 20 business days of receipt of the notice of non-compliance.
- The payer must review the EVV Usage Score for the following quarter from the date of the notice of non-compliance requiring EVV training.
- If the minimum EVV Usage Score is met, no further action will be taken by the payer for the compliant quarter.
- If the minimum EVV Usage Score is not met, the payer may document and apply a CAP.
- The payer must review the EVV Usage Score for the following quarter from the date of the notice of non-compliance requiring EVV training.
- Two or more occurrences within a 24-month period - Require completion of a CAP within ten business days of receipt of the notice of non-compliance
- The payer must review the EVV Usage Score for the following quarter from the date of implementation of an accepted CAP.
- If the minimum EVV Usage Score is met, no further action will be taken by the payer for the compliant quarter.
- If the minimum EVV Usage Score is not met, the payer may initiate contract termination.
- The payer must review the EVV Usage Score for the following quarter from the date of implementation of an accepted CAP.
- Three or more occurrences within a 24-month period - Propose to terminate contract
- Payers cannot terminate a contract unless:
- The payers have followed the above progressive enforcement actions.
- The program provider or FMSA has not met the minimum EVV Usage Score for a total of three quarters (nine months) within in a 24-month period.
- Payers cannot terminate a contract unless:
When the program provider or FMSA fails to complete training or CAP requirements as explained above, the payer may temporarily withhold Medicaid claims payments until requirements are met.
Before a payer enforcing action, payers must do their due diligence and ensure failure to meet and maintain the compliance score was not due to:
- Payer errors such as:
- Late authorizations
- Missing or incorrect HCPCS, Modifiers, Service Group and Service Codes provided by the payer
- A system outage, defect or issue related to the EVV Aggregator, EVV Portal or an EVV Vendor System
- Natural disasters
CDS Employer Enforcement Actions
When a CDS employer fails to meet and maintain the minimum EVV Usage score in a state fiscal year quarter, the payer may send a notice of non-compliance to enforce one or more of the following progressive enforcement actions based on the number of occurrences within a 24-month period:
- First occurrence within a 24-month period - Require additional EVV policy and system trainings within a specific time frame
- The payer must review the EVV Usage Score for the following quarter from the date of the notice of non-compliance requiring additional EVV training.
- If the minimum EVV Usage Score is met, the payer takes no further action for the compliant quarter.
- If the minimum EVV Usage Score is not met, the payer may document and apply a corrective action plan (CAP).
- The payer must review the EVV Usage Score for the following quarter from the date of the notice of non-compliance requiring additional EVV training.
- Two or more occurrences within a 24-month period - Require completion of a CAP with assistance from the FMSA within ten business days of the notice of non-compliance
- The payer must review the EVV Usage Score for the following quarter from the date of implementation of an accepted CAP.
- If the minimum EVV Usage Score is met, the payer takes no further action for the compliant quarter.
- If the minimum EVV Usage Score is not met, the payer may recommend removal from the CDS option.
- The payer must review the EVV Usage Score for the following quarter from the date of implementation of an accepted CAP.
- Three or more occurrences within a 24-month period - Recommend removal from the CDS option
Before a payer enforcing action, payers must do their due diligence and ensure failure to meet and maintain the compliance score was not due to:
- FMSA administrative errors
- A system outage, defect or issue related to the EVV Aggregator, EVV Portal, an EVV Vendor System or an EVV Proprietary System
- Natural disasters
FMSAs are responsible for facilitating communication between payers and CDS employers related to EVV compliance including but not limited to delivering:
- Notices of non-compliance from a payer to a CDS employer
- Responses from a CDS employer back to the payer
Review Period Schedule
The EVV usage review period schedule follows the state fiscal year quarters. Payers may begin reviews any time after the visit maintenance time frame has expired for the specified state fiscal year quarter.
EVV Usage Review Period Schedule
| Quarter Number | Review Period and State Fiscal Year Quarters Based on Date of Service | EVV Usage Review Dates |
|---|---|---|
| 1 | September, October, November | After the visit maintenance time frame has expired from the last date of the specified quarter, Nov. 30. |
| 2 | December, January, February | After the visit maintenance time frame has expired from the last date of the specified quarter, Feb. 28. or Feb. 29 if during a leap year. |
| 3 | March, April, May | After the visit maintenance time frame has expired from the last day of the specified quarter, May 31. |
| 4 | June, July, August | After the visit maintenance time frame has expired from the last day of the specified quarter, Aug. 31. |
EVV Usage Report
Payers will use the EVV Usage Report located in the EVV Portal to conduct EVV Usage Reviews for visits with a date of service within the Review Period.
Program providers and FMSAs have access to the EVV Usage Report in the EVV Portal.
FMSAs have access to the EVV FMSA Usage Report in the EVV Portal.
FMSAs and CDS employers have access to the EVV CDS Employer Usage Report in the EVV Portal and EVV system.
Refer to 13000 Reports for more information.
State-Required Personal Care Services Grace Period
EVV Usage Reviews begin any time after the visit maintenance time frame has expired from the last day of the specified state fiscal year quarter. The grace period dates of service started Sept. 1, 2019 and ended Aug. 31, 2020 for these services.
Cures Act Personal Care Services Grace Period
EVV Usage Reviews begin after:
- The visit maintenance time frame has expired.
- The grace period has ended.
- The grace period dates of service started Jan. 1, 2021 and ended on Dec. 31, 2021 for program providers and FMSAs.
- Due to availability of the EVV CDS Employer Usage report, the grace period dates of service for CDS employers started Jan. 1, 2021 and end Aug. 31, 2022 unless noted by HHSC.
10020 EVV Landline Phone Verification Reviews
Revision 22-4; Effective Sept. 1, 2022
Payers review the phone number used for clocking in and clocking out of the EVV system to ensure the phone number is from an allowable phone type.
Refer to 7000 Clock In and Clock Out Methods for more information.
Failure to Meet the Compliance Standard
Failure to meet required actions outlined in 7030 Home Phone Landline and in the notice of non-compliance sent by the payer may result in the payer temporarily withholding Medicaid claims payments from the program provider or FMSA until compliance is met.
If the FMSA is unable to meet required actions due to a CDS employer not meeting required actions outlined in 7030 Home Phone Landline, the FMSA must notify the payer immediately in writing by email or fax.
Program Provider and FMSA Enforcement Actions
When the program provider or FMSA fails to meet required actions within 20 business days of the notice of non-compliance sent by the payer, the payer may temporarily withhold Medicaid claims payments from the program provider or FMSA.
Payers will remove the temporary withholding of Medicaid claims payments within two business days of receiving acceptable documentation as outlined in the notice of non-compliance sent by the payer and described in 7030 Home Phone Landline.
CDS Employer Enforcement Actions
When the CDS employer fails to meet required actions within 10 business day of notification by the FMSA:
- The FMSA can remove the unallowable landline phone type from the EVV system as the member’s home phone landline, and
- The FMSA can follow TAC 40, Part 1, Chapter 41, Subchapter B, Rule Section 41.221 relating to failure to submit complete service delivery documentation or meeting CDS employer responsibilities and place the CDS employer on a CAP.
Review Period Schedule
EVV Landline Phone Verification Reviews will be at the payer’s discretion. It may occur any time after the date of the visit if the phone number used to clock in and clock out has already been captured in the EVV system.
Refer to 7000 Clock In and Clock Out Methods for more information.
EVV Landline Phone Verification Report
Payers will use the EVV Landline Phone Verification Report located in the EVV system to conduct EVV Landline Phone Verification Reviews.
Program providers, FMSAs and CDS employers who have selected Option 1 or 2 on Form 1722, Employers Selection for Electronic Visit Verification Responsibilities, have access to the EVV Landline Phone Verification Report in the EVV system.
CDS employers who selected Option 3 on Form 1722, Employers Selection for Electronic Visit Verification Responsibilities, must establish a process to get the EVV Landline Phone Verification Report with their FMSA. This does not apply if the CDS Employer has read only access to the EVV system. Contact your FMSA for more information.
Refer to 13000 Reports for more information.
State-Required Personal Care Services Grace Period
There is no grace period for EVV Landline Phone Verification Reviews. Reviews may occur any time after the date of the visit if the phone number used to clock in and clock out has already been captured in the EVV system.
Cures Act Personal Care Services Grace Period
EVV Landline Phone Verification Reviews will begin after the grace period has ended. The grace period dates of service started Jan. 1, 2021 and ended on Dec. 31, 2021.
10030 EVV Required Free Text Reviews
Revision 22-4; Effective Sept. 1, 2022
Payers will review EVV visit transactions to determine if required free text is entered when using a reason code.
Failure to document any required free text may result in recoupment of associated claim(s).
Refer to 9000 EVV Reason Code for more information.
Note: For the CDS option, as of Jan. 1, 2022 payers will not conduct Required Free Text Reviews until further notice as determined by HHSC.
Failure to Meet Compliance Standard
Program providers and FMSAs who fail to ensure required free text is entered into the EVV system prior to submitting an EVV claim may have associated claims recouped.
Review Period Schedule
The review period occurs any time after the visit maintenance time frame has expired and at the payer’s discretion.
EVV Reason Code Usage and Free Text Report or EVV Visit Log Report
Payers will use the EVV Reason Code Usage and Free Text Report or the EVV Visit Log Report (located in the EVV Portal) to conduct EVV Required Free Text Reviews.
Program providers and FMSAs must use the EVV Reason Code Usage and Free Text Report or the EVV Visit Log Report (located in the EVV Portal) to monitor compliance of required free text.
Refer to 13000 Reports for more information.
State-Required Personal Care Services Grace Period
There is no grace period for EVV Required Free Text Reviews. Reviews may begin any time after the visit maintenance time frame has expired.
Cures Act Personal Care Services Grace Period
EVV Required Free Text Reviews will begin after:
- The visit maintenance time frame has expired
- The grace period has ended
- The grace period started Jan. 1, 2021 and ended on Dec. 31, 2021
10040 HHSC EVV Informal Reviews and MCO Disputes
Revision 22-4; Effective Sept. 1, 2022
HHSC EVV Informal Reviews
Program providers, FMSAs and CDS employers
Program providers, FMSAs and CDS employers may request an informal review of EVV Compliance Review results for re-examination if they:
- disagree with the EVV compliance review findings provided by HHSC; and
- believe the review did not adhere to current HHSC EVV TAC and policies.
EVV Informal Reviews are:
- Conducted to re-examine the disputed results
- Conducted by HHSC EVV Operations staff who were not involved in the review under question
- Completed within 20 business days of the request receipt date
The EVV Informal Reviews process includes the following activities:
- Acknowledgment of receipt through email of the EVV Informal Reviews request
- Establishing the informal review team
- Conducting the EVV Informal Reviews
- Notifying the program provider, FMSA, or CDS employer in writing of the EVV Informal Reviews results
The results of the EVV Informal Review are final.
Requesting an EVV Informal Review
Program providers, FMSAs, or CDS employers may request EVV Informal Reviews within 10 business days after receipt of the notice of non-compliance by submitting a secure email request to the EVV Compliance inbox.
The request must include:
- The notice of non-compliance and the quarterly EVV Usage Report.
- Explanation of the basis for believing the EVV Compliance Review was not conducted according to TAC and EVV policies
- Any supporting documentation such as:
- Any relevant communication with TMHP, EVV vendors, payers, FMSAs or CDS employers
- Documentation of relevant EVV system issues
- Any other documentation that supports the program provider’s, FMSA’s, or CDS employer’s disagreement with the EVV Compliance Review results
Failure to follow the steps above will result in HHSC denying the EVV Informal Review request.
MCO Disputes
Program providers, FMSAs and CDS employers
Program providers, FMSAs and CDS employers may request a dispute of the EVV Compliance Review results for re-examination with their MCO if they:
- disagree with the EVV compliance review findings provided by an MCO; and
- believe the review did not adhere to current HHSC EVV TAC and policies.
Contact your MCO for instructions on how to dispute the EVV Compliance Review results.
10050 Formal Appeal of HHSC Enforcement Actions
Revision 22-4; Effective Sept. 1, 2022
Per Texas Administrative Code Title 1, Part 15, Chapter 357, Subchapter I, Rule Section 357.484 program providers, FMSAs or CDS employers may request an administrative hearing in writing within 15 days after receipt of the notice of non-compliance if appealing the withholding of Medicaid claims payments.
Send the written request to:
Texas Health and Human Services Commission
Legal Services
Office of General Counsel
P.O. Box 149030
Mail Code W-615
Austin, Texas 78714
Fax: 512-438-5759
11000, Usage
Revision 22-4; Effective Sept. 1, 2022
Program providers, FMSAs and CDS employers are required to use an EVV system and meet the minimum EVV Usage Score.
Payers will monitor the number of manually entered EVV visit transactions and the number of rejected EVV visit transactions to ensure the minimum EVV Usage Score is met for the state fiscal year quarter.
Refer to 10000 EVV Compliance Reviews for more information.
A manually entered EVV visit transaction is an EVV visit that is manually entered into the EVV system when a service provider or CDS employee fails to use the EVV system to clock in when service delivery begins, clock out when service delivery ends, or both.
Refer to 7000 Clock In and Clock Out Methods for more information.
A rejected EVV visit transaction is an EVV visit transaction that is exported from an EVV system to the EVV Aggregator but is not accepted by the EVV Aggregator.
11010 EVV Usage Score
Revision 22-4; Effective Sept. 1, 2022
Program Providers
Program providers must achieve and maintain a minimum EVV Usage Score of 80% rounded to the nearest whole percentage, each state fiscal year quarter, unless noted by HHSC.
Program providers below the EVV Usage Score will be reviewed. Payers may choose to review all program providers or a sample of program providers that did not meet the minimum EVV Usage Score.
Score Calculations
The EVV Usage Score for a program provider equals the Manual EVV Visit Transaction Score plus the Rejected EVV Visit Transaction Score.
The Manual EVV Visit Transaction Score equals the number of total electronic (non-manual) visit transactions divided by the total number of accepted visit transactions by the EVV Aggregator and then multiplied by 60 percent.
The Rejected EVV Visit Transaction Score equals the number of non-rejected visit transactions divided by the total number of exported visit transactions sent to the EVV Aggregator and then multiplied by 40 percent.
Non-rejected visit transactions are the number of visit transaction submission attempts that were not rejected.

FMSAs
FMSAs must achieve and maintain a minimum EVV Usage score of 80% rounded to the nearest whole percentage, each state fiscal year quarter, unless noted by HHSC.
FMSAs below the EVV Usage Score will be reviewed. Payers may choose to review all FMSAs or a sample of FMSAs that did not meet the minimum EVV Usage Score.
Score Calculations
The EVV Usage Score, for an FMSA, equals the Rejected EVV Visit Transaction Score.
The Rejected EVV Visit Transaction Score equals the number of non-rejected visit transactions divided by the total number of exported visit transactions sent to the EVV Aggregator.
Non-rejected visit transactions are the number of visit transaction submission attempts that were not rejected.

CDS Employers
CDS Employers must achieve and maintain a minimum EVV Usage Score of 80% rounded to the nearest whole percentage, each state fiscal year quarter, unless noted by HHSC. See table below for CDS employer EVV Usage Score requirements based on service delivery dates.
CDS employers below the EVV Usage Score will be reviewed. Payers may choose to review all CDS employers or a sample of CDS employers that did not meet the minimum EVV Usage Score.
| Fiscal Year (FY) | Quarter (Q) | Service Delivery Dates | EVV Usage Score |
|---|---|---|---|
| FY 23 | Q1 | 9/1/2022 – 11/30/2022 | 40% |
| FY 23 | Q2 | 12/01/2022 – 2/28/2023 | 60% |
| FY 23 | Q3 | 3/1/2023 – ongoing | 80% |
Score Calculations
The EVV Usage Score, for a CDS employer, equals the Manual EVV Visit Transaction Score.
The Manual EVV Visit Transaction Score equals the number of total electronic (non-manual) visit transactions divided by the total number of accepted visit transactions by the EVV Aggregator.

11020 Manual EVV Visit Transaction Score
Revision 22-4; Effective Sept. 1, 2022
The Manual EVV Visit Transaction Score:
- Excludes manual EVV visit transactions with zero bill hours
- Includes manual EVV visit transactions accepted by the EVV Aggregator
- Only counts a manual EVV visit transaction one time
- When an EVV visit transaction is manually entered into the EVV system or an EVV visit transaction is missing a clock in or a clock out time which must be manually entered into the EVV system, the EVV visit transaction counts against the Manual EVV Visit Transaction Score once.
Refer to 7000 Clock In and Clock Out Methods for more information.
11030 Rejected EVV Visit Transaction Score
Revision 22-4; Effective Sept. 1, 2022
When an EVV visit transaction is sent to the EVV Aggregator and does not pass all EVV visit transaction validations, the EVV visit transaction is rejected and sent back to the EVV system. This is to notify the program provider, FMSA or CDS employer visit maintenance is required.
Each time a visit transaction is rejected by the EVV Aggregator, it counts against the Rejected EVV Visit Transaction Score. This is true for EVV visits which are exported from an EVV system and rejected by the EVV Aggregator multiple times.
For example:
- On Monday a program provider submits an EVV visit transaction to the EVV Aggregator, and the EVV visit transaction is rejected.
- On Tuesday, the program provider completes visit maintenance and resubmits the EVV visit transaction to the EVV Aggregator. The EVV Aggregator rejects the EVV visit transaction again.
- On Wednesday, the program provider completes visit maintenance and resubmits the EVV visit transaction to the EVV Aggregator. The EVV Aggregator accepts the EVV visit transaction.
- In this scenario the Rejected EVV Visit Transaction Score will reflect:
- Two rejected EVV visit transactions
- One non-rejected EVV visit transaction
- Three total exported EVV visit transactions
A rejected EVV visit transaction only counts against the Rejected EVV Visit Transaction Score if the rejection is identified as a program provider or FMSA error.
The following table shows data elements, as applicable, and EVV visit transaction rejection reasons identified as program provider or FMSA errors that count as a rejected EVV visit transaction.
| Edit Number | Data Elements (as applicable) | EVV Visit Rejection Reason |
|---|---|---|
| Ex0002C | NPI | Provider NPI cannot be validated as active for the visit date. |
| Ex0003C1 | API | Provider API cannot be validated as active for the visit date. |
| Ex00031C | Payer | The Member's Payer on the EVV visit does not match our records for this Member. |
| Ex00034C1 | Member Medicaid ID | The member Medicaid ID on the EVV visit is not found in our records. |
| Ex00034C2 | Member Medicaid ID (no active eligibility) | The member Medicaid ID on the EVV visit does not have active Medicaid eligibility for the visit date. |
| Ex00043C | MCO Member Service Delivery Area (SDA) | The MCO member SDA on the EVV visit does not match the Plan Code associated with the member's payer. |
| Ex00057C1 | Service Group and Service Code combination | The service group and service code combination on the EVV visit are not eligible for EVV. |
| Ex00057C2 | Service Group not valid for Provider Number | The service group and Service Code combination on the EVV visit are not valid for the Provider number on the visit. |
| Ex00057C3 | Member not authorized for Service Group/Service Code combination | The member on the EVV visit is not authorized for this service group/service code on this visit date in our records. |
| Ex00059C | HCPCS and Modifier combination not eligible for EVV | The HCPCS Code and EVV Modifier combination on the EVV visit is not eligible for EVV. |
Refer to the TMHP EVV website to access the EVV Visit Transaction Rejection Guide which explains all rejection reasons.
11040 How EVV Usage Reviews are Conducted
Revision 22-4; Effective Sept. 1, 2022
Payers conduct EVV Usage Reviews by the following contract and agreement types:
- Program providers and FMSAs with LTC FFS contracts are monitored at the provider number level.
- Example: If a program provider or FMSA has five different LTC FFS contracts, each unique provider number will receive an EVV Usage Score.
- Program providers and FMSAs enrolled with TMHP for Acute Care FFS are monitored at the NPI or API/TIN combination level.
- Example: If a program provider or FMSA has three different NPIs or APIs with the same TIN or three different TINs, each NPI or API/TIN combination will receive an EVV Usage Score whether the TIN is the same or different.
- Program providers and FMSAs with MCO contracts are monitored at the NPI or API/TIN combination level.
- Example: If a program provider or FMSA has three different NPIs or APIs with the same TIN or three different TINs, each NPI or API/TIN combination will receive an EVV Usage Score whether the TIN is the same or different.
- CDS employers are monitored at the member level.
- Example: Each member who has selected the CDS option will be reviewed.
12000, EVV Claims
Revision 21-1; Effective Nov. 1, 2021
The program provider or FMSA must only submit claims for reimbursement once all the visits for the claim line items have been completed and accepted in the EVV Aggregator. The EVV Aggregator will perform a claims match against the accepted EVV visit transactions stored in the EVV Portal.
The payer must not pay a claim without a matching accepted EVV visit transaction stored in the EVV Portal.
12100 Claims Submission
Revision 22-2; Effective Mar. 1, 2022
All EVV services listed in the EVV Service Bill Codes Table on the HHSC EVV webpage are subject to this policy.
Each claims management system will forward the EVV claims to the EVV Aggregator for the EVV claims matching process. The EVV Aggregator will return the EVV claims and the EVV claims match result code(s) back to the claims management system for further claims processing.
Program providers and FMSAs must:
- Follow the billing guidelines of their payer, either HHSC or their MCO, when submitting an EVV claim.
- Submit EVV claims per claim line item with either a single date of service or a span of dates as required by their payer billing guidelines. Refer to 12200 Claims Matching for more information about how the EVV Aggregator performs the EVV claims match for each type of billing.
- Notify the third-party submitter of 12100 Claims Submission when using a third-party claims submitter or billing agent,
- Submit EVV claims for the program and services as detailed in the tables below.
- Meet all timely filing requirements.
LTC FFS
Program providers and FMSAs must submit EVV claims for LTC FFS to the TMHP Claims Management
System for the following program and services:
| Program | Services | Service Delivery Options |
|---|---|---|
| Community Attendant Services (CAS) |
|
|
| Community Living Assistance and Support Services (CLASS) Waiver |
|
|
| Deaf Blind with Multiple Disabilities (DBMD) Waiver |
|
|
| Family Care (FC) |
|
|
| Primary Home Care (PHC) |
|
|
| HCS Waiver |
|
|
| TxHmL Waiver |
|
|
Acute Care FFS
Program providers and FMSAs must submit EVV claims for Acute Care FFS to the TMHP Compass 21 (C21) system for the following programs and services:
| Program | Services | Service Delivery Options |
|---|---|---|
| Personal Care Services (PCS) |
|
|
| Community First Choice (CFC) |
|
|
YES
Program providers must submit EVV Claims for YES to the HHSC Clinical Management for Behavioral Health Services (CMBHS) system for the following program service:
| Program | Services | Service Delivery Options |
|---|---|---|
| YES Waiver | In-Home Respite |
|
HCBS-AMH Waiver
Program providers must submit EVV claims for HCBS-AMH to HHSC using an Encounter Invoice Template for the following program services:
| Program | Services | Service Delivery Options |
|---|---|---|
| HCBS-AMH Waiver |
|
|
Managed Care Long-Term Services and Supports (LTSS)
Program providers and FMSAs must submit EVV claims to TMHP C21 for the following managed care programs and services:
| Program | Services | Service Delivery Options |
|---|---|---|
| STAR Health |
|
|
| STAR Health – Medically Dependent Children’s Program (MDCP) Covered Services |
|
|
| STAR Kids |
|
|
| STAR Kids – MDCP Covered Services |
|
|
| STAR+PLUS |
|
|
| STAR+PLUS – Home and Community Based Services (HCBS) |
|
|
| STAR+PLUS - Medicare-Medicaid Plan (MMP) |
|
|
Access the EVV Contact Information Guide (PDF) on the HHSC EVV webpage to determine who to contact for other questions about the EVV claims submission process.
Program providers and FMSAs can access TMHP’s EDI homepage for basic information needed to submit claims electronically including:
- User guides
- Forms
- Technical information intended for billing agents that file claims on behalf of program providers and FMSAs
12200 Claims Matching
Revision 21-1; Effective Nov. 1, 2021
All EVV claims for services required to use EVV must match to an accepted EVV visit transaction in the EVV Aggregator (the state’s centralized EVV database) before reimbursement of an EVV claim by the payer. TMHP, the claims administrator for the state of Texas, oversees this process.
Payers will deny or recoup an EVV claim that does not match an accepted EVV visit transaction. This includes fee-for-service claims paid by HHSC, acute care claims paid by TMHP on behalf of HHSC and managed care claims paid by the MCO.
Program providers and FMSAs using a third party to bill claims must notify the third party of 12200 Claims Matching.
12210 Claims Matching Process
Revision 21-1; Effective Nov. 1, 2021
HHSC uses the EVV claims matching process to identify one or more EVV visits that support a Medicaid claim. Once a program provider or FMSA submits an EVV claim to a claims management system operated by HHSC or TMHP, the claims management system forwards any claims for EVV services to the EVV Aggregator for the claims matching process.
The automated claims matching process includes:
- Receiving an EVV claim line item.
- Matching data elements from each EVV claim line item to data elements from one or more accepted EVV visit transactions in the EVV Aggregator.
- Forwarding an EVV claim match result code to the payer once the claims match process is complete.
Program providers and FMSAs must use the EVV Portal to review and confirm the EVV Aggregator has accepted the EVV visit transactions before submitting the EVV claim(s) for those services.
The following data elements from the claim line item and the EVV visit transaction must match:
| EVV Claim Line Item | Accepted EVV Visit Transaction |
|---|---|
| Medicaid ID | Medicaid ID |
| Date of Service | EVV Visit Date |
| National Provider Identifier (NPI) or Atypical Provider Identifier (API) | NPI or API |
| Healthcare Common Procedure Coding System (HCPCS) Code | HCPCS Code |
| HCPCS Modifiers | HCPCS Modifiers |
| Billed Units | Billable Units (if applicable) |
If any of the above data elements do not match, the claim matching process will return an unsuccessful match result code and the payer will deny the claim.
The EVV claims matching process supports EVV claims submitted with a single date of service and EVV claims submitted with a span of service dates.
Unit Matching for Multiple Visits on the Same Date of Service
If there are multiple visits for the same member for the same service (HCPCS and Modifier combination) from the same provider on the same date of service, the claims matching process combines the total number of units on all accepted EVV visits for that date and compares the unit total to the billed units on the claim line item.
Unit Matching Requirement for EVV Claims with Single Line Item
Program providers and FMSAs submitting EVV claims with a single EVV claim line item for each date of service must have one or more matching accepted EVV visit transactions for the same date in the EVV Aggregator or the payer may deny or recoup the EVV claim line item.
Unit Matching Requirement for EVV Claims with Span Dates (more than one consecutive date)
Program providers and FMSAs submitting an EVV claim with a span of dates for a line item must ensure that:
- Each date of service within the span of dates has one or more matching EVV visit transactions accepted in the EVV Aggregator.
- The total units on the EVV claim line item must match the combined total units on the accepted EVV visit transactions for the span of dates, if applicable.
The payer will deny or recoup an EVV claim line item with span dates that does not meet the above criteria.
12220 Exceptions to the Claims Matching Process
Revision 21-1; Effective Nov. 1, 2021
HHSC will establish any exceptions to the claims matching process in the EVV Service Bill Codes Table.
Service-Specific Bypass
HHSC will bypass the claims matching process for specific services. Refer to the EVV Service Bill Codes Table for the specific services that bypass the claims matching process.
Units Matching Bypass
The EVV claims matching process does not match units on the EVV visit transaction against the billed units on the EVV claim line item for any of the services associated with the CDS option.
In addition, the claims matching process does not match units on the EVV visit transactions against the billed units on the claim line item for other specific services. Refer to the EVV Service Bill Codes Table for the specific services that bypass the units matching process.
Bypass for Disasters and Temporary Circumstances
HHSC may temporarily set the EVV claims matching process to bypass EVV claims in response to a disaster or temporary circumstances that may disrupt delivery of services. In such cases, HHSC will provide written direction to program providers and FMSAs, including the effective dates of the bypass.
12230 Claims Match Result Codes
Revision 22-4; Effective Sept. 1, 2022
Claims Match Result Codes are codes used to indicate if an EVV claim line item matched or did not match to an accepted EVV visit transaction.
Based on the result of the claims matching process, the EVV Portal displays a claims match result code and the EVV Aggregator returns the claims match result code to the claims management system for final claims processing.
The claims match result codes viewable in the EVV Portal are:
- EVV01 – EVV Successful Match
- EVV02 – Medicaid ID Mismatch
- EVV03 – Visit Date Mismatch
- EVV04 – Provider (NPI/API) or Attendant ID Mismatch
- EVV05 – Service Mismatch (HCPCS and Modifiers if applicable)
- EVV06 – Units Mismatch
- EVV07 – Match Not Required
- EVV08 – Natural Disaster
Payers will communicate the results of the final claims processing to program providers and FMSAs.
Claims Match Result Code EVV01
If the EVV Aggregator identifies one or more accepted EVV visit transactions matching the EVV claim line item, the claims matching process will return an EVV01 – EVV Successful Match result code.
Payers may still deny or recoup an EVV claim with a claims match result code EVV01 if other claim requirements fail the claims adjudication process.
For example:
- Payers may deny an EVV claim if the amount billed exceeds the authorized amount for the member.
- Payers may recoup an EVV claim if the program provider or FMSA changes EVV visit data after an EVV visit transaction matched and an updated EVV claim is not submitted by the program provider or FMSA.
Claims Match Result Codes EVV02 – EVV06
If the EVV Aggregator identifies a mismatch between an accepted EVV visit transaction and an EVV claim line item, the claims matching process will return one of the claims match result codes of EVV02, EVV03, EVV04, EVV05 or EVV06.
The payer will deny an EVV claim if the EVV claim line item receives a claims match result code of EVV02, EVV03, EVV04, EVV05 or EVV06.
Claims Match Result Codes EVV07 and EVV08
When HHSC implements a bypass of the claims matching process for a disaster or other temporary circumstance the claims matching process will return claims match result codes of EVV07 or EVV08.
Payers will not deny an EVV claim with EVV07 or EVV08 claims match result codes for an unsuccessful match.
Payers may still deny an EVV claim with claims match result codes EVV07 or EVV08 if other claim requirements fail the claims adjudication process.
When HHSC bypasses the claims matching process, the EVV Aggregator will still perform the claims matching process between the EVV claim line item and the EVV visit transaction to record the actual claims match results. Program providers and FMSAs can view the actual claims match results in the EVV Portal to determine whether the EVV claim would have matched without the bypass.
Payers may recoup the EVV claim if the program provider or FMSA does not follow instructions from the payer related to claims match result codes EVV07 or EVV08.
Claims Status Report
Payers will return a claims status report for each EVV claim. The claims status report includes claims match result codes and the final claims processing result. This may include an Explanation of Benefit (EOB), Explanation of Payment (EOP) or a Denial Claims Report. Claims status reports differ by the payer and program.
See the table below for the claims management system responsible for reporting EVV claims status.
| Payer | Claims Management System | Claims Status Reports |
|---|---|---|
| TMHP on behalf of HHSC (Acute Care FFS) | TMHP Compass 21 | Remittance and Status (R&S) Report |
| HHSC (LTC FFS) | TMHP Claims Management System | R&S Report |
| Managed Care | MCO Claims Systems | Varies |
| HHSC (YES) | CMBHS Claims System | R&S Report |
| HHSC (HCBS-AMH) | Encounter Invoice Template | HHSC-AMH |
Refer to the Contact Information Guide on the HHSC EVV webpage for who to contact with questions about the claims matching process or EVV claim denials.
13000, Reports
Revision 22-2; Effective March 1, 2022
The EVV Reports Policy covers EVV standard reports that HHSC and MCOs use for oversight and data analysis, such as but not limited to:
- EVV compliance reviews
- Contract monitoring
- Recoupment
- Fraud, waste and abuse reviews
Program providers and FMSAs must access the HHSC EVV standard reports located in the EVV Portal and EVV systems.
CDS employers must access HHSC EVV standard reports in the EVV system.
13010 EVV Portal Standard Reports
Revision 23-1; Effective Jan. 6, 2023
Below are the EVV standard reports available to program providers, FMSAs, MCOs and state staff in the EVV Portal.
EVV Service Provider History Report
- Verifies which service providers and CDS employees provided services to a member for a requested date range.
EVV Claim Match Reconciliation Report
- EVV01 Report:
- Identifies claims that received a match code of EVV01 at the time of the claims matching process and receive a different match code on the report run date.
- Displays the match code the claim would receive on the report run date. These include match codes EVV02, EVV03, EVV04, EVV05, EVV06, EVV07 or EVV08.
- Serves as a tool for program providers, FMSAs and payers to research claim matching codes.
- EVV07 or EVV08 Report:
- Identifies claims that received a match code of EVV07 or EVV08 and an informational match code of EVV02, EVV03, EVV04, EVV05 or EVV06 at the time of the claims matching process.
- Displays the match code the claim would receive on the report run date. These include match codes EVV01, EVV02, EVV03, EVV04, EVV05 or EVV06.
- Serves as a tool for program providers, FMSAs and payers to research informational claim matching codes.
EVV CDS Employer Usage Report
- Displays the EVV Usage Score for the preceding quarter(s), for each Medicaid member that selects the CDS option with HHSC or an MCO.
- Used by payers to determine the EVV Usage Score and conduct EVV Usage Reviews.
- Allows CDS employers to monitor the EVV Usage compliance requirement. Refer to 10000 EVV Compliance Reviews and 11000 Usage for more information.
EVV Service Provider Clock In and Clock Out Report
- Displays the service provider’s and CDS employee’s:
- Use of EVV clock in and clock out methods.
- Total visits worked within a specific date range.
- Percentage of total visits worked for each clock in and clock out method within a specific date range.
EVV Provider Report
- Displays contract or enrollment data used by the program provider or FMSA during setup in the EVV system.
- Displays the program provider or FMSA EVV system onboarding date, start date and end date.
EVV Reason Code Usage and Free Text Report
- Used to conduct EVV compliance reviews for reason code and required free text. Refer to 10000 EVV Compliance Reviews for more information.
- Displays the EVV reason code number, reason code description and any free text entered on accepted EVV visits transactions during a specified month, sorted by each program provider’s or FMSAs unique identifier.
- Allows program providers and FMSAs, on behalf of the CDS employers, to search reason code usage and enters free text by Medicaid ID.
EVV Units of Service Summary
- Displays daily, weekly and monthly totals of services delivered for a Medicaid ID.
- Allows for identifying breaks in service for a Medicaid ID.
EVV Usage Report
- Used to conduct EVV usage reviews. Refer to 10000 EVV Compliance Reviews and 11000 EVV Usage for more information.
- Displays the EVV Usage Score for each program provider and FMSA for the preceding quarter(s).
EVV Visit Log
- Displays the hours of service delivered by the service provider or CDS employee to the member.
- Includes all EVV accepted visit data sent to the EVV Aggregator for service delivery visits on or after Sept. 1, 2019.
- Displays the:
- Schedule, if applicable.
- Actual hours.
- Location.
- EVV clock in and clock out method for each visit.
13020 EVV System Standard Reports
Revision 23-1; Effective Jan. 6, 2023
Below are the EVV system standard reports available to program providers, FMSAs, CDS employers, MCOs and state staff in the EVV system.
EVV Alternative Device Order Status Report
- Used to verify and track the status of alternate devices orders.
EVV Service Provider History*
- Verifies which service providers and CDS employees provided services to a member for a requested date range.
EVV CDS Service Delivery Log
- Displays EVV visit data for CDS employers for a requested date range.
- Data is based only on completed and verified visits from the EVV system.
EVV CDS Employer Usage Report
- Displays the EVV Usage Score for the preceding quarter(s), for each Medicaid member that selects the CDS option with HHSC or an MCO.
- Used by payers to determine the EVV Usage Score and conduct EVV Usage Reviews.
- Allows CDS employers to monitor the EVV Usage compliance requirement. Refer to 10000 EVV Compliance Reviews and 11000 Usage for more information.
EVV Service Provider Clock In and Clock Out Report*
- Displays the service provider’s and CDS employee’s:
- Use of EVV clock in and clock out methods.
- Total visits worked within a specific date range.
- Percentage of total visits worked for each clock in and clock out method within a specific date range.
EVV Landline Phone Verification Report
- Used to conduct EVV compliance landline phone reviews. Refer to 10000 EVV Compliance Reviews for more information.
- Displays the phone number used for clocking in and clocking out of the EVV system to ensure the home phone landline number is an allowable phone type.
EVV Reason Code Usage and Free Text Report*
- Used to conduct EVV compliance reviews for reason code and required free text. Refer to 10000 EVV Compliance Reviews for more information.
- Displays the EVV reason code number, EVV reason code description and any free text entered on accepted EVV visits transactions during a specified month, sorted by each program provider’s or FMSAs unique identifier.
- Allows program providers and FMSAs, on behalf of the CDS employers, to search reason code usage and enters free text by Medicaid ID.
EVV Service Delivery Exception Report
- Shows the number of visits that varied from the schedule or authorization, as well as the number of visits that were not approved, for a requested date range.
- Data must include services regardless of service delivery locations including home or community location, and ‘GPS’ coordinates when the mobile method is used to clock in and clock out.
EVV Units of Service Summary*
- Displays daily, weekly and monthly totals of services delivered for a Medicaid ID.
- Identifies breaks in service for a Medicaid ID.
Non-EVV Relevant Time Logged Report
- Displays service provider and CDS employee time spent on non-EVV services during each visit for a requested date range.
*The report is exported from the EVV Portal.
13030 EVV Vendor Ad Hoc Reporting
Revision 21-1; Effective November 1, 2021
Ad hoc reports are EVV non-standard reports. HHSC and MCOs will not use ad hoc reports for contract oversight monitoring or compliance reviews.
The EVV vendor, or EVV PSO where applicable, must provide ad hoc reporting of any EVV data available in the EVV system at no additional cost to HHSC, MCOs, program providers, FMSAs or CDS employers.
Contact your EVV vendor or EVV PSO with questions about ad hoc reporting.
13040 EVV Portal Search Tools
Revision 22-2; Effective March 1, 2022
HHSC, MCOs, program providers and FMSAs can perform the following searches for EVV visit transactions in the EVV Portal.
Accepted Visit Search
- Displays the current accepted EVV visit transactions within a specific date range.
Visit History Search
- Allows users to search for EVV visit transactions that have been accepted or rejected by the EVV aggregator.
- Search results display all changes made to an EVV visit transaction through visit maintenance in the EVV system; including EVV visit transactions rejections and the EVV rejection code(s).
EVV Claim Search
- Allows users to search for EVV claims.
- Search results display EVV claims, claims match result codes and other claim information.
- Claims with a claim mismatch result codes will not have an EVV Visit ID because the EVV Aggregator was unable to match those claims to a visit.
For questions about:
- EVV standard reports in the EVV Portal, contact EVV@TMHP.com.
- EVV standard reports in the EVV system, contact your EVV vendor or EVV PSO.
- EVV policy, contact your payer.
14000, Non-EVV Services
Revision 22-4; Effective Sept. 1, 2022
A non-EVV service is an authorized service that is not required to use EVV.
Program providers, FMSAs and CDS employers must continue to follow program documentation requirements for non-EVV services.
Using the EVV system does not replace paper documentation for non-EVV services.
The program provider, FMSA or CDS employer will determine how the service provider or the CDS employee will clock in and clock out of the EVV system when delivering non-EVV services and EVV services throughout the day.
Based on the option chosen by the program provider or FMSA and CDS employer, the service provider or CDS employee will use one of the following options to document a non-EVV service that occurs during an EVV visit:
- Option 1: Clock in to the EVV system and clock out of the EVV system before the non-EVV service begins and clock back in to the EVV system after the non-EVV service has ended.
- Option 2: Remain clocked in to the EVV system while delivering the non-EVV service and document the amount of time spent on the non-EVV service. Note: Follow the EVV vendor or PSO instructions on how to subtract the non-EVV service time at the end of the EVV visit and use appropriate Reason Code Numbers and Reason Code Descriptions as necessary.
Examples for recording non-EVV time
The service provider or CDS employee is working from 8 a.m. to 2 p.m. The service provider or CDS employee spends five hours on EVV services from 8 a.m. – noon and 1 – 2 p.m. and one hour on non-EVV services from noon – 1 p.m.
- Option 1: Clock in to the EVV system and clock out of the EVV system before the non-EVV service begins and clock back in to the EVV system after the non-EVV service has ended.
- The service provider or CDS employee will:
- Clock in to the EVV system at 8 a.m. and clock out at noon
- Begin the non-EVV service
- Clock back in to the EVV system at 1 p.m. and clock out at 2 p.m.
- Document the non-EVV services in accordance with program policy
- The service provider or CDS employee will:
- Option 2: Remain clocked in to the EVV system while delivering the non-EVV service and document the amount of time spent on the non-EVV service.
- The service provider or CDS employee will:
- Clock in to the EVV system at 8 a.m. and clock out at 2 p.m.
- Document the non-EVV service in accordance with program policy.
- The program provider, FMSA or CDS employer will use the EVV system to document one hour of non-EVV services.
- Contact your EVV vendor or PSO for instruction on how to adjust the bill hours.
- The service provider or CDS employee will:
Program providers, FMSAs and CDS employers can review the reported non-EVV service time by accessing the Non-EVV Relevant Time Logged Report in the EVV system. The report will show the total hours worked for non-EVV services.
Note: Program providers, FMSAs or CDS employers must contact their EVV vendor or PSO to determine how to document non-EVV services for members with pre-scheduled visits.
15000, Fraud Waste and Abuse
Revision 22-2; Effective March 1, 2022
If the payers determine that a program provider, FMSA or CDS employer is not compliant with EVV policy and procedures, it could result in a referral for a fraud, waste, and abuse investigation.
If you are made aware of, or suspect situations that may be considered Medicaid fraud, waste, or abuse, report it to the HHSC Inspector General online or by calling their toll-free fraud hotline at 800-436-6184.
16000, EVV CDS Employer Policies
Revision Notice 22-3; Effective June 1, 2022
This section provides important EVV policies and identifies sections in the EVV Policy Handbook for CDS employers. CDS employers must read 16000 EVV CDS Employer Policies and the EVV Policy Handbook sections identified throughout this section to review all EVV policies relevant to CDS employers.
EVV CDS employer policies provide EVV standards and policy requirements that CDS employers and Medicaid members who selected the CDS option must follow if receiving a service required to use EVV.
EVV requirements apply to programs and services identified in HHSC TAC Title 1, Part 15, Chapter 354, Subchapter O, Rule Section 354.4005, Applicability. They are listed in the Programs and Services Required to Use EVV table located on the EVV webpage.
For EVV services provided on or after Jan. 1, 2021, CDS employers must ensure CDS employees clock in and clock out of the EVV system. Refer to 7000 Clock In and Clock Out Methods for more information.
CDS employers must use the EVV system selected by their FMSA. Contact your FMSA to determine which EVV system your FMSA uses.
If CDS employees do not use the EVV system, or if CDS employers do not comply with EVV requirements:
- CDS employees may experience a delay in payment or inaccurate payments
- CDS employers must take more training
- An FMSA may require CDS employers to complete a corrective action plan in accordance with TAC 40, Part 1, Chapter 41, Subchapter B, Rule Section 41.221
- CDS employers may be subject to removal from the CDS option
- EVV claims payments without an accepted EVV visit transaction may be denied or recouped.
Refer to 10000 EVV Compliance Reviews and 15000 Fraud, Waste and Abuse for more information.
To avoid these consequences, contact your FMSA immediately. Begin using the EVV system as soon as possible.
CDS employers must complete Form 1722, Employer’s Selection for Electronic Visit Verification Responsibilities to select how they will participate in EVV. All CDS employers, regardless of what option they select on the form, must:
- Ensure CDS employees use the EVV system to clock in when EVV services begin and clock out when EVV services end.
- Approve CDS employee time worked in a timely manner.
CDS employers must continue to follow program rules regarding documentation requirements. EVV does not change applicable federal and state laws related to documentation requirements. FMSAs, CDS employers and CDS employees must comply with applicable federal and state laws related to confidentiality of a member’s information.
16010 CDS Option Stakeholders
Revision Notice 22-3; Effective June 1, 2022
The following are stakeholders in the CDS option and must meet all state and federal EVV requirements.
The FMSA contracts with HHSC or an MCO (payer) to provide financial management services to CDS employers.
The FMSA is responsible for:
- Payroll and budget management
- Selecting an EVV system
- Adding and maintaining member, CDS employer and CDS employee information into the EVV system
- Adding and maintaining member service authorizations into the EVV system
- Creating the username and temporary password for CDS employers
- Creating the username and temporary password for CDS employees
- Assisting the CDS employer with completing, and updating Form 1722, Employer’s Selection for EVV Responsibilities and entering selections into the EVV system
- Training CDS employers on EVV policy
- The CDS employer also has the option to take EVV policy training with their payer
- Helping CDS employers with questions related to EVV policy and process
- Confirming approved time worked in the EVV system to ensure the services and hours were authorized
The CDS Employer is a member or legally authorized representative (LAR) responsible for hiring and retaining a service provider who delivers a Medicaid service to a member.
CDS employers are responsible for:
- Completing all required EVV training.
- Training CDS employees on the use of the EVV system.
- Ensuring CDS employees use the EVV system to clock in when services begin and clock out when services end.
- Approving time worked.
- Signing up for GovDelivery to receive the most current news and alerts related to EVV
A Designated Representative (DR) is a person designated by the CDS employer to support or assist with meeting CDS employer responsibilities.
CDS employers can appoint a DR to assist or to perform EVV responsibilities in the CDS option using CDS Form 1720, Appointment of a Designated Representative. However, CDS employers still retain responsibility for CDS requirements.
CDS employers will specify which EVV tasks the DR will assist with or handle. Tasks might include approving CDS employee time worked or training CDS employees. CDS employers are responsible for actions taken by the DR.
The Legally Authorized Representative (LAR) is a person authorized by law to act on behalf of a parent, guardian or managing conservator of a minor, or the guardian of an adult.
The CDS Employee is a person who provides Medicaid services and is employed or contracted by a CDS employer.
The member is a person receiving Medicaid services.
Members are responsible for:
- Reviewing and signing the form EVV Responsibilities and Additional Information.
- Notifying their FMSA if a CDS employee asks the member to clock in or clock out of the EVV system.
16020 CDS Employer Steps Prior to Using an EVV System
Revision Notice 22-3; Effective June 1, 2022
CDS employers must complete the following steps before using an EVV system:
Step 1: Complete Form 1722, Employer’s Selection for EVV Responsibilities with FMSA assistance.
Step 2: Complete all required EVV trainings (Refer to 4230 EVV Training Requirements for CDS Employers):
- EVV System
- EVV Policy
Step 3: Train CDS employees on the clock in and clock out methods. (Refer to 4240 Training Requirements for Service Providers and CDS Employees)
Form 1722, Employer’s Selection for EVV Responsibilities
With assistance from the FMSA, CDS employers must complete this form by choosing the appropriate option for using the EVV system.
CDS employers may choose to have the DR assist with EVV responsibilities described on Form 1722, Employer’s Selection for EVV Responsibilities, if the CDS employer appoints a DR. The CDS employer is responsible for any actions taken by the DR and must ensure that the DR follows all privacy and security protocols, including when the DR accesses EVV data.
CDS employers who selected Option 1 (Option 1 CDS employer) on Form 1722, Employer’s Selection for Electronic Visit Verification Responsibilities must:
- Ensure they have access to the EVV system and can perform EVV responsibilities.
- Ensure CDS employees use the EVV system to clock in when EVV services begin and clock out when EVV services end.
- Complete visit maintenance in the EVV system within the visit maintenance time frame.
- Approve CDS employee time worked in the EVV system in a timely manner.
CDS employers who selected Option 2 (Option 2 CDS employer) on Form 1722, Employer’s Selection for Electronic Visit Verification Responsibilities must:
- Ensure CDS employees use the EVV system to clock in when EVV services begin and clock out when EVV services end.
- Approve CDS employee time worked in the EVV system in a timely manner.
CDS employers who selected Option 3 (Option 3 CDS employer) on Form 1722, Employer’s Selection for Electronic Visit Verification Responsibilities must:
- Ensure CDS employees use the EVV system to clock in when EVV services begin and clock out when EVV services end.
- Approve CDS employee time worked using the method the FMSA and CDS employer have agreed to in a timely manner.
- Refer to program policy, CDS policy or the FMSA for more information.
If time worked is not captured in the EVV system, Medicaid cannot reimburse the FMSA for payroll. CDS employees may experience a delay in payment.
CDS employers must provide Form 1722, Employer’s Selection for EVV Responsibilities, to the FMSA.
If the CDS employer does not complete and provide Form 1722, Employer’s Selection for EVV Responsibilities to the FMSA before the member starts receiving EVV services, the FMSA will select Option 3 when creating the CDS employer’s account in the EVV system. CDS employers can request a change by completing a form and providing it to the FMSA.
Refer to Form 1722, Employer's Selection for Electronic Visit Verification Responsibilities for more information.
Required Training for CDS Employers
EVV Policy Handbook 4200 EVV Training requires CDS employers, or the appointed DR, to complete all required EVV training prior to using an EVV system for the first time and yearly.
Refer to 4230 EVV Training Requirements for CDS Employers for more information.
CDS employers can access HHSC EVV Training Requirements Checklist to track training requirements and completion of requirements. The checklist is available on the EVV Training Resources webpage.
CDS Employer Training Responsibilities
CDS employers are responsible for providing Clock In and Clock Out Methods training to CDS employees.
CDS employers must use Form 1732, Management and Training of Service Provider to keep up-to-date training records of CDS employee training completions. CDS employers must provide Form 1732 to the FMSA.
Refer to 4240 Training Requirements for Service Providers and CDS Employees for more information.
System Access for the CDS Employer
The FMSA is responsible for creating a username and temporary password in the EVV system for CDS employers depending on the option selected on Form 1722, Employer’s Selection for EVV Responsibilities:
- Option 1: As needed for EVV system training, completing visit maintenance and approving time worked in the EVV system.
- Option 2: As needed for EVV system training and approving time worked in the EVV system.
- Option 3: As needed for EVV system training overview. Check with your FMSA to request view or read only access.
The EVV system or the FMSA will send CDS employers a username and the temporary password.
If the CDS employer is not the member, the FMSA will include the CDS employer’s information in the member profile and provide the username and temporary password to the CDS employer.
If the member has a DR, both the CDS employer and the DR will each have a unique username and temporary password.
CDS employers will use the username and temporary password to log in to the EVV system and change the temporary password.
The FMSA can only see the CDS employer’s username and email address in the EVV system. However, both the FMSA and the CDS employer can change the CDS employer’s password.
If the CDS employer does not receive a username and temporary password for any reason, contact the FMSA.
System Access for the CDS Employee
The FMSA is responsible for creating a username and temporary password for the CDS employee.
The FMSA or the CDS employer provides the username and temporary password to the CDS employee. CDS employers must contact the FMSA to determine who will provide the CDS employee the username or temporary password.
If the CDS employee does not receive a username and temporary password for any reason, contact the FMSA or the CDS employer.
Information Updates
CDS employers are responsible for ensuring payers and the FMSA have the most up to date information in the EVV system.
CDS employers must communicate to the FMSA if any of the following information changes:
- Payer(s)
- FMSA
- Member’s address
- Member’s home phone landline number, if applicable
- Member’s and CDS Employer’s contact information
- CDS employees
Schedules
EVV policy does not require the entry of schedules into the EVV system. Service delivery can occur with or without a schedule.
For members in the CDS option, schedules are optional to enter in the EVV system.
Some Medicaid programs require the use of a schedule for service delivery. FMSAs and CDS employers must follow the member’s program requirements to determine if schedules are required in the EVV system.
If the CDS employer wants to use schedules in the EVV system or the program requires a schedule, CDS employers must work with their FMSA to determine how schedules will be entered.
Refer to 4600 Schedules for more information.
16030 CDS Employer(s) Using an EVV System
Revision Notice 22-3; Effective June 1, 2022
Once CDS employers have completed Steps 1 -3 in 16020 CDS Employer Steps Prior to Using an EVV System, they can use the EVV system.
The following steps explain when to use the EVV system and required actions for CDS employers.
Step 4: The CDS employer must ensure the CDS employee uses an approved clock in and clock out method to:
- Clock in at the beginning of service delivery.
- Clock out at the end of service delivery.
Step 5: Option 1 CDS employers, or an FMSA on behalf of Option 2 and Option 3 CDS employers, must complete visit maintenance to:
- Correct any exceptions or critical errors.
- Adjust bill hours, if needed.
- Add Reason Codes as required.
- Enter manual EVV visits, if necessary.
Step 6: CDS employers must review and approve time worked after visit maintenance is complete.
- Option 1 and Option 2 CDS employers will approve time worked using the EVV system.
- Option 3 CDS employers will approve time worked using the method the FMSA and CDS employer have agreed to in a timely manner.
Visit Maintenance
Visit maintenance is the process used by the FMSA or CDS employer to correct the identification and visit data in the EVV system to accurately reflect the delivery of service.
Option 1 CDS employers must complete visit maintenance using the EVV system and must refer to section 8000 Visit Maintenance for detailed EVV policy requirements.
Option 1 CDS employers must:
- Verify the EVV system captured data correctly.
- Complete visit maintenance if there are exceptions or critical errors on an EVV visit transaction.
- Use the most appropriate EVV Reason Code Number(s), EVV Reason Code Description(s) and free text, if applicable. Refer to 9000 EVV Reason Code for more information.
- Enter manual EVV visits, if necessary.
Option 2 and Option 3 CDS employers elected to have their FMSA complete visit maintenance. Option 2 and Option 3 CDS employers must work with their FMSA to provide any necessary information for the FMSA to complete visit maintenance in a timely manner.
Approving Time Worked
After visit maintenance is complete and the EVV visit transaction accurately reflects time worked, CDS employers must approve time worked.
Option 1 CDS employers must verify the EVV system captured data correctly and complete visit maintenance before using the EVV system to approve time worked.
Option 2 CDS employers must work with their FMSA to ensure all required data elements are correct and visit maintenance is complete before Option 2 CDS employers approve time worked using the EVV system.
Option 3 CDS employers must review and approve time worked using the method the FMSA and CDS employer have agreed to in a timely manner.
Failure to approve CDS employee time worked in a timely manner may result in:
- CDS employees experiencing a delay in payment or inaccurate payments.
- CDS employers taking additional required training.
16040 Failure to Use an EVV System in the CDS Option
Revision Notice 22-3; Effective June 1, 2022
CDS employers:
- Must ensure an approved EVV system is used to document the delivery of EVV-required services.
- Are responsible for ensuring CDS employees use the EVV system to clock in when services begin and clock out when services end.
If the CDS employee does not use the EVV system to clock in or clock out, for any reason, they must document service delivery information and submit the documentation to the FMSA or CDS employer.
Option 1 CDS employers must manually enter the visit into the EVV system and keep all service delivery documentation.
Option 2 and Option 3 CDS employers must provide service delivery documentation to the FMSA to ensure visits are manually entered into the EVV system by the FMSA. The FMSA or CDS employer must keep service delivery documentation.
Refer to 1400 Failure to use an EVV System, 7000 Clock In and Clock Out Methods and 11000 Usage for more information.
16050 CDS EVV Compliance
Revision Notice 22-3; Effective June 1, 2022
CDS employers:
- Are responsible for meeting compliance requirements for EVV Usage and EVV Landline Phone Verification.
- Have access to system standard reports in the EVV system and must monitor compliance reports monthly, at a minimum.
Refer to 10000 EVV Compliance Reviews, 11000 Usage and 13020 EVV System Standard Reports for more information.
16060 CDS Bonuses and Overtime
Revision Notice 22-3; Effective June 1, 2022
EVV does not change, impact or track:
- Bonuses in the CDS option
- Overtime in the CDS option
Follow your FMSA’s process for bonuses and overtime.
16070 CDS Complaints
Revision Notice 22-4; Effective Sept. 1, 2022
CDS employers who have complaints may contact:
- CDS@hhs.texas.gov for complaints about a delay in payment from an FMSA or for general CDS program requirement complaints related to EVV.
- EVV@hhs.texas.gov for general complaints about EVV requirements.
- HHSC Office of the Ombudsman for escalation of a complaint.
CDS employers can find the EVV Contact Information Guide for CDS Employers under resources on the EVV Consumer Directed Services Option webpage.
Appendices
Appendix I, EVV Reason Codes Table
Revision 21-1; Effective November 1, 2021
Refer to the EVV webpage for the most up to date EVV Reason Codes and Free Text requirements.
Appendix II, Historical Alerts and Archived Policies
Revision 22-2; Effective March 1, 2022
Forms
Revisions
23-1, Handbook Changes
22-4, Handbook Changes
Revision Notice 22-4; Effective Sept. 1, 2022
The following change(s) were made:
| Section | Title | Change |
|---|---|---|
| 1200 | State Laws and Rule | Updates section title and text. |
| 1600 | Key Terms | Updates key terms. |
| 2100 | Payers | Updates text. |
| 2300 | EVV Vendors | Updates text. |
| 2400 | EVV Proprietary System Operator | Updates text. |
| 2500 | Program Provider | Updates text. |
| 2600 | Financial Management Services Agency | Updates text. |
| 2700 | Member | Updates text. |
| 2800 | CDS Employer | Updates text. |
| 3000 | Programs and Services Required to Use EVV | Updates text. |
| 4000 | EVV System and Setup | Updates text. |
| 4110 | EVV Vendor Systems | Updates text. |
| 4120 | EVV Proprietary Systems | Updates text. |
| 4130 | Select an EVV System | Updates text. |
| 4200 | EVV Training | Updates text. |
| 4500 | Service Authorizations | Updates text. |
| 4700 | EVV System Transfer | Updates text. |
| 4710 | Transferring EVV Systems | Previously section 4720. Updates title and text. Title is now How to Transfer to an EVV Vendor System. |
| 4720 | How to Transfer to an EVV Vendor in the State Vendor Pool | Previously section 4730. Updates title and text. Title is now How to Transfer to an EVV Proprietary System. |
| 4730 | How to Transfer to an EVV Proprietary System | Deletes section. |
| 5000 | EVV Proprietary System | Updates text. |
| 5010 | Eligibility to Use an EVV Proprietary System | Previously section 5020. Updates title and text. Title is now Reimbursement for Use of an EVV Proprietary System. |
| 5020 | Reimbursement for Use of an EVV Proprietary System | Previously section 5030. Updates title and text. Title is now EVV Proprietary System Operator Responsibilities. |
| 5030 | EVV Proprietary System Operator Responsibilities | Previously section 5040. Updates title and text. Title is now EVV Proprietary System Onboarding Process. |
| 5040 | EVV Proprietary System Onboarding Process | Previously section 5050. Updates title and text. Title is now EVV Proprietary System Operational Readiness Review. |
| 5050 | EVV Proprietary System Operational Readiness Review | Previously section 5060. Updates title and text. Title is now Success or Failure of the Operational Readiness Review. |
| 5060 | Success or Failure of the Operational Readiness Review | Previously section 5070. Updates title and text. Title is now EVV Proprietary System General Operations. |
| 5070 | EVV Proprietary System General Operations | Previously section 5080. Updates title and text. Title is now Access to the EVV Proprietary System. |
| 5080 | Access to the EVV Proprietary System | Previously section 5100. Updates title and text. Title is now Proprietary System Operator Compliance. |
| 5090 | Required EVV Proprietary System Standard Reports | Deletes section. |
| 5100 | Proprietary System Operator Compliance Reviews | Deletes section. |
| 5200 | HHSC Cancellation of EVV Proprietary System Approval | Deletes section. |
| 5300 | Transferring EVV Systems | Deletes section. |
| 5400 | Proprietary System Fraud, Waste and Abuse | Deletes section. |
| 6000 | EVV Visit Transaction | Updates text. |
| 6100 | EVV System | Updates text. |
| 7000 | Clock In and Clock Out Methods | Updates text. |
| 7010 | Manually Entered EVV Visits | Updates text. |
| 7020 | Mobile Method | Updates text. |
| 7040 | Alternative Device | Updates text. |
| 7050 | Using Multiple Clock In and Clock Out Methods | Updates text. |
| 7060 | EVV Services Delivered Outside the Member’s Home | Updates text. |
| 8000 | Visit Maintenance | Updates text. |
| 8010 | Required Visit Maintenance | Updates text. |
| 8020 | Exceptions and Schedules | Updates section title and text. |
| 8050 | Visit Maintenance Time Frame | Updates text. |
| 8060 | Visit Maintenance Unlock Request | Updates text. |
| 8070 | Visit Maintenance and Billing EVV Claims | Updates text. |
| 9000 | EVV Reason Code | Updates text. |
| 10000 | EVV Compliance Reviews | Updates text. |
| 10010 | EVV Usage Reviews | Updates text. |
| 10020 | EVV Landline Phone Verification Reviews | Updates text. |
| 10030 | EVV Required Free Text Reviews | Updates text. |
| 10040 | HHSC EVV Informal Reviews and MCO Disputes | Updates text. |
| 10050 | EVV Formal Appeal of the Review | Updates section title and text. |
| 11000 | Usage | Updates text. |
| 11010 | EVV Usage Score | Updates text. |
| 11020 | Manually Entered EVV Visit Transactions | Updates section title and text. |
| 11030 | Rejected EVV Visit Transactions | Updates section title and text. |
| 11040 | EVV Usage Reviews | Updates section title and text. |
| 11050 | Compliance | Deletes section |
| 12230 | Claims Match Result Codes | Updates text. |
| 14000 | Non-EVV Services | Updates text. |
| 16070 | CDS Complaints | Updates CDS inbox. |
22-3, Handbook Changes
Revision Notice 22-3; Effective June 1, 2022
The following change(s) were made:
| Section | Title | Change |
|---|---|---|
| 4600 | Schedules | Updates text |
| 4610 | Schedule Types | Adds new subsection |
| 8100 | Visit Maintenance Reduction Features | Updates text |
| 16000 | EVV CDS Employer Policies | Adds new subsection |
| 16010 | CDS Option Stakeholders | Adds new subsection |
| 16020 | CDS Employer Steps Prior to Using an EVV System | Adds new subsection |
| 16030 | CDS Employer(s) Using an EVV System | Adds new subsection |
| 16040 | Failure to Use an EVV System in the CDS Option | Adds new subsection |
| 16050 | CDS EVV Compliance | Adds new subsection |
| 16060 | CDS Bonuses and Overtime | Adds new subsection |
| 16070 | CDS Complaints | Adds new subsection |
22-2, Handbook Changes
Revision Notice 22-2; Effective March 1, 2022
The following change(s) were made:
| Section | Title | Change |
|---|---|---|
| 1600 | Key Terms | Updates text and adds new terminology |
| 4000 | EVV System and Setup | Updates text |
| 4120 | EVV Proprietary Systems | Updates text |
| 4130 | EVV Training | Updates text |
| 4200 | EVV Training Requirements for FMSAs | Updates text |
| 4220 | EVV Training Requirements for CDS Employers | Updates text |
| 4230 | Training Requirements for Service Provider and CDS Employees | Updates text |
| 4240 | Data Collection | Adds web link and title of Form 1732 |
| 4400 | Service Authorizations | Updates text |
| 4500 | Transferring EVV Systems | Updates text |
| 4710 | How to Transfer to an EVV Vendor in the State Vendor Pool | Updates language |
| 4720 | How to Transfer to an EVV Vendor in the State Vendor Pool | Updates title and language |
| 4730 | How to Transfer to an EVV Proprietary System | Updates language |
| 5000 | EVV Proprietary System | Updates language |
| 5030 | EVV Proprietary System Operator Responsibilities | Updates language and includes new PSO approval paths |
| 5040 | EVV Proprietary System Onboarding Process | Updates text |
| 5050 | EVV Proprietary System Operational Readiness Review | Updates title, text and language |
| 5060 | Success or Failure of the Operational Readiness Review | Updates title, text and language |
| 5070 | EVV Proprietary System General Operations | Updates text and language |
| 5100 | Proprietary System Operator Compliance Reviews | Updates title and text |
| 5200 | HHSC Cancellation of EVV Proprietary System Approval | Updates text |
| 5300 | Transferring EVV Systems | Updates text and language |
| 5400 | Proprietary System Fraud, Waste and Abuse | Updates title, text and language |
| 10010 | EVV Usage Reviews | Updates text and language |
| 12100 | Claims Submission | Updates text and LTC FFS table |
| 12230 | Claims Match Result Codes | Updates text and EVV04 description |
| 13000 | Reports | Updates text |
| 13010 | EVV Portal Standard Reports | Updates text and adds EVV CDS Employer Usage Report |
| 13020 | EVV System Standard Reports | Updates text and adds EVV CDS Employer Usage Report |
| 13040 | EVV Portal Search Tools | Updates TMHP EVV email address |
| 15000 | Fraud, Waste and Abuse | Updates text and adds FMSAs and CDS employers |
| Appendices | Appendices | Updates text and adds FMSAs and CDS employers
|
EVV Contact Us
For technical or accessibility issues with this handbook, email: form.handbook.request@hhs.texas.gov
For questions about Electronic Visit Verification Provider Policy Handbook, please email: EVV@hhs.texas.gov.